Keratotic nodular and/or papular lesions affecting the hands may correspond to different entities that share clinical and histopathologic findings. The lesions include degenerative collagenous and elastotic plaques of the hands, nodular amyloidosis, colloid milium, acrokeratoelastoidosis, focal-acral hyperkeratosis, and punctate palmoplantar keratoderma. The last 3 conditions differ from the others in that no frank deposits are seen in histopathology.
A 70-year-old Mexican man (resident in Mexico) was assessed for lesions affecting the upper limbs. His history was remarkable for a nonspecified degenerative joint disease and untreated prostatic hyperplasia. He also reported occasionally taking ibuprofen and omeprazole.
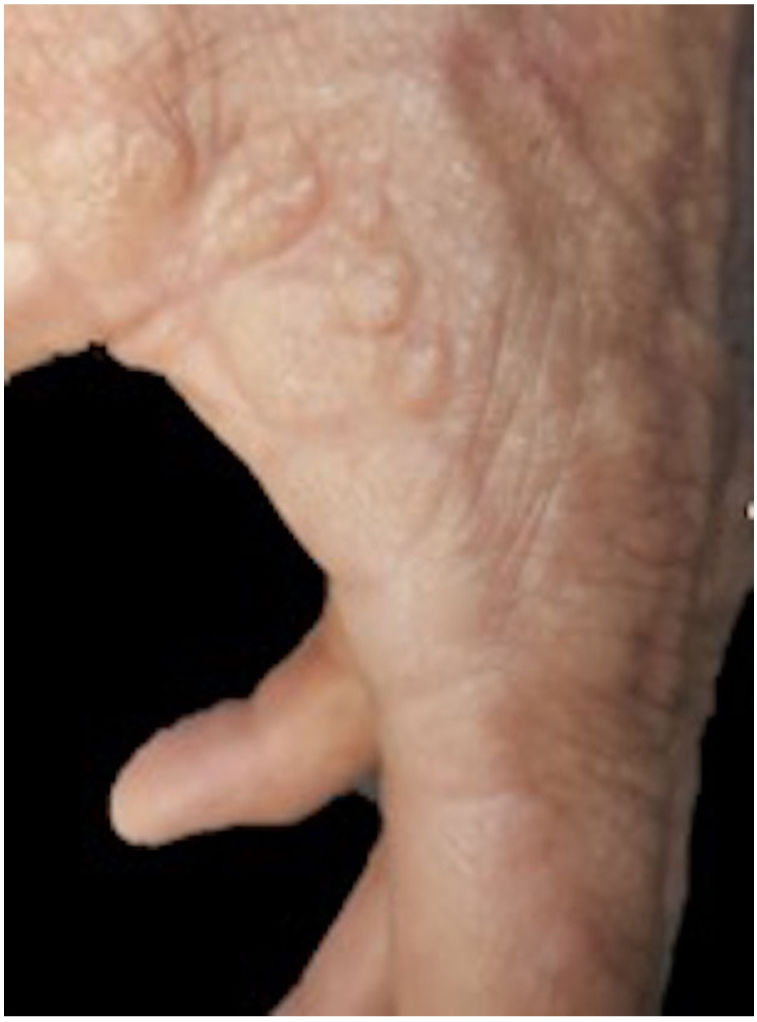
Examination revealed a symmetrical rash affecting the dorsum and the edge of the palm of both hands. The lesion comprised yellowish nodules measuring 2–12mm in diameter. These were well demarcated, yellowish in color, and of firm consistency. The patient reported them to be asymptomatic (Fig. 1). He had used topical sunscreen and taken topical retinoic acid 0.05% for 2 years, albeit with no response.
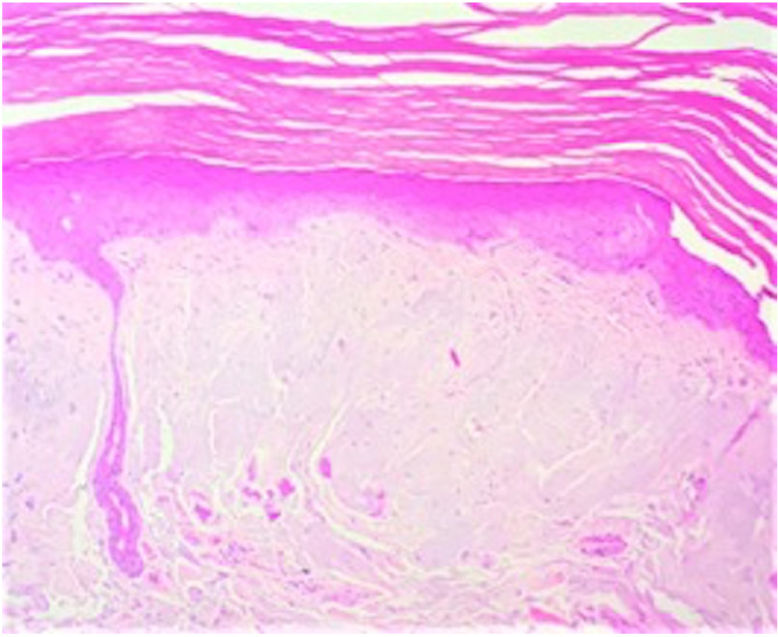
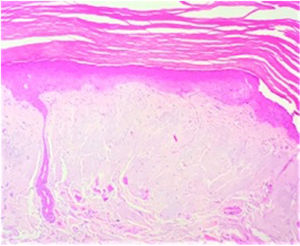
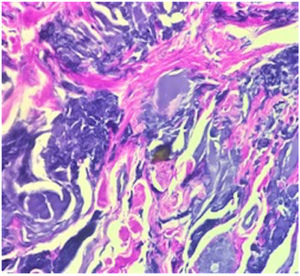
The initial diagnosis was colloid milium or acrokeratoelastoidosis. The histology workup of a punch biopsy specimen taken from one of the lesions revealed an epidermis with irregular acanthosis of the interpapillary ridges and a hyperkeratotic stratum compactum. The papillary and superficial dermis were characterized by deposition of abundant eosinophilic material. This was smooth with clefts, surrounded some blood vessels, and was separated from the epidermis by a Grenz zone. A moderate perivascular inflammatory infiltrate composed mainly of lymphocytes was visible in the superficial and mid dermis (Fig. 2). No sweat gland abnormalities were observed.
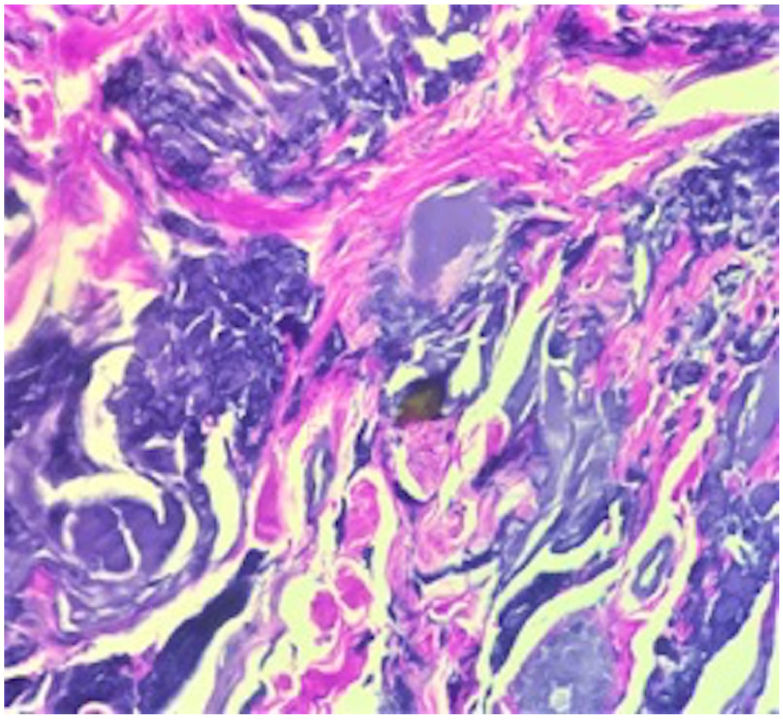
The deposit was stained with periodic acid–Schiff and Verhoeff–van Gieson and Grocott, which stain elastic fibers (Fig. 3). Crystal violet staining was focally positive. Immunohistostaining for the κ and λ chains was negative.
The patient received 3 cryotherapy sessions, which partially improved the lesion.
Nodular and papular lesions of the hands pose a diagnostic challenge owing to the multiple clinical conditions the dermatologist and histopathologist must address. The differential diagnosis includes degenerative collagenous and elastotic plaques of the hands, an uncommon condition first described in 1960 by Burks et al.1 and that is characterized by the presence of keratotic translucent papules at the juncture of the palmar and dorsal skin.2 It has been associated with UV radiation and repetitive injury.1 The very few cases that have been reported are referred to by different names and histopathologic presentations. The lesions are found mainly on the internal margin of the thumb, from where they extend to the edge of the interdigital space and the radial aspect of the index finger.3 Histologically, they are characterized by the presence of numerous thickened collagen bundles interlaced with elastic fibers and an amorphous basophilic material in the reticular dermis.4
The differential diagnosis also includes colloid milium, a rare cutaneous deposition disorder that was first described in 1866 by Wagner.5 While the exact etiology remains unknown, it is thought to result from degeneration of collagen and elastic fibers after prolonged sun exposure, leading to the formation of protein residue clusters.6 The 4 subtypes of colloid milium comprise adult, juvenile, nodular, and pigmented. The adult type is the most common and is characterized clinically by multiple papules that differ in size and are yellowish-pink in color. They are symmetrical and slow-growing and generally affect sun-exposed areas, such as the face, neck, and hands.7 Considered essential for diagnosis, histopathology reveals pale, homogeneous, amorphous cleaved eosinophilic material located in the papillary dermis with a background of solar elastosis.6 Adult colloid milium stains positive for periodic acid–Schiff and Congo red, although the reaction for the latter is weaker.8
Nodular amyloidosis is an uncommon form of primary cutaneous amyloidosis, in which amyloid material comes from immunoglobulin light chains produced by plasma cells. It is a differential diagnosis for nodular lesions affecting the hands. Clinically, it is characterized by yellowish-brown plaques, papules, or nodules that appear on the head, trunk, arms, legs, and genitals.9 Histopathology reveals large amyloid deposits in the dermis and subcutaneous cellular tissue accompanied by a perivascular lymphoplasmacytic infiltrate. The amyloid material stands out in light chain immunohistochemistry.10 Special stains are generally necessary to distinguish between colloid milium and nodular amyloidosis. Van Gieson staining can prove helpful, since it stains the colloid material yellow and the amyloid material red. Electron microscopy is the definitive test for distinguishing between both conditions.9
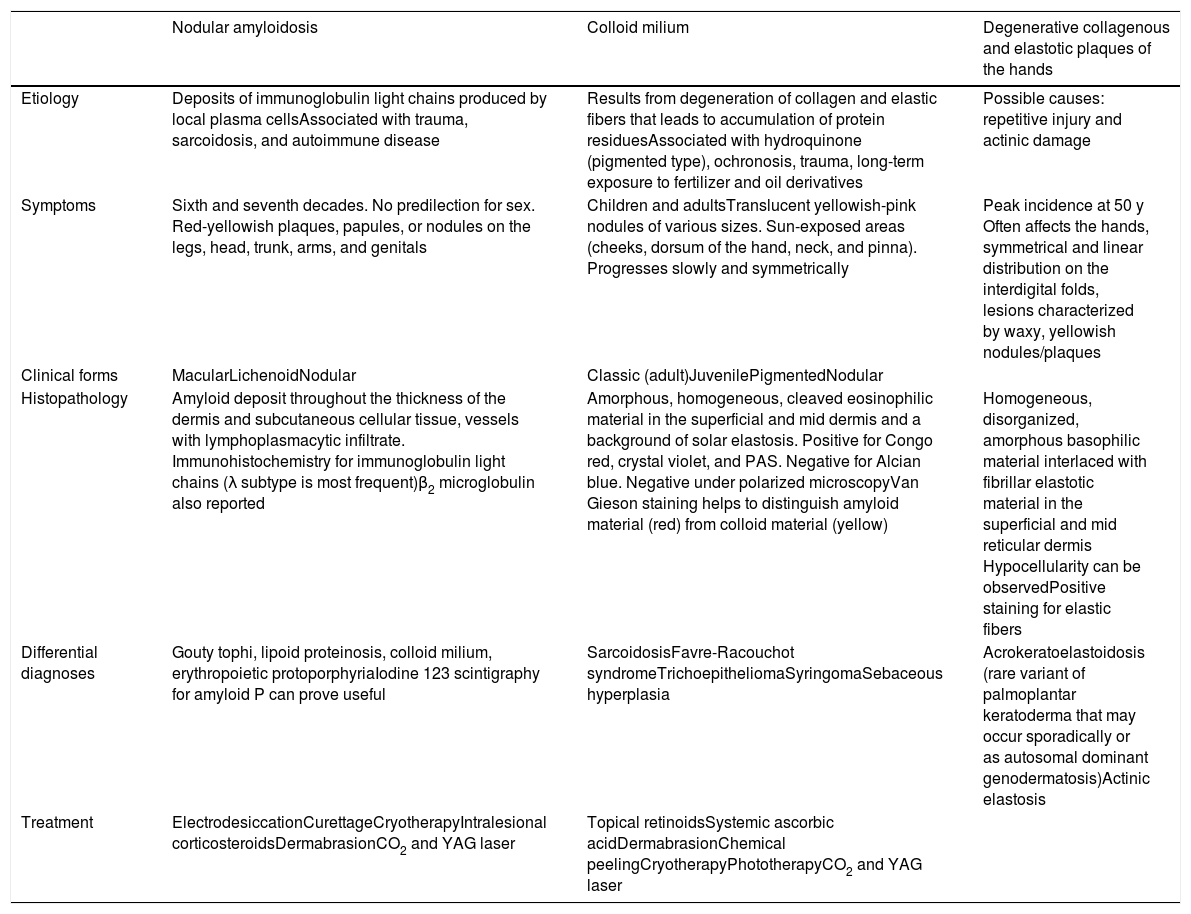
Table 1 summarizes the clinical, histopathologic, and therapeutic differences between all 3 entities.
Clinical, Histopathologic, and Treatment-Related Differences in Acral Dermatosis.
| Nodular amyloidosis | Colloid milium | Degenerative collagenous and elastotic plaques of the hands | |
|---|---|---|---|
| Etiology | Deposits of immunoglobulin light chains produced by local plasma cellsAssociated with trauma, sarcoidosis, and autoimmune disease | Results from degeneration of collagen and elastic fibers that leads to accumulation of protein residuesAssociated with hydroquinone (pigmented type), ochronosis, trauma, long-term exposure to fertilizer and oil derivatives | Possible causes: repetitive injury and actinic damage |
| Symptoms | Sixth and seventh decades. No predilection for sex. Red-yellowish plaques, papules, or nodules on the legs, head, trunk, arms, and genitals | Children and adultsTranslucent yellowish-pink nodules of various sizes. Sun-exposed areas (cheeks, dorsum of the hand, neck, and pinna). Progresses slowly and symmetrically | Peak incidence at 50 y Often affects the hands, symmetrical and linear distribution on the interdigital folds, lesions characterized by waxy, yellowish nodules/plaques |
| Clinical forms | MacularLichenoidNodular | Classic (adult)JuvenilePigmentedNodular | |
| Histopathology | Amyloid deposit throughout the thickness of the dermis and subcutaneous cellular tissue, vessels with lymphoplasmacytic infiltrate. Immunohistochemistry for immunoglobulin light chains (λ subtype is most frequent)β2 microglobulin also reported | Amorphous, homogeneous, cleaved eosinophilic material in the superficial and mid dermis and a background of solar elastosis. Positive for Congo red, crystal violet, and PAS. Negative for Alcian blue. Negative under polarized microscopyVan Gieson staining helps to distinguish amyloid material (red) from colloid material (yellow) | Homogeneous, disorganized, amorphous basophilic material interlaced with fibrillar elastotic material in the superficial and mid reticular dermis Hypocellularity can be observedPositive staining for elastic fibers |
| Differential diagnoses | Gouty tophi, lipoid proteinosis, colloid milium, erythropoietic protoporphyriaIodine 123 scintigraphy for amyloid P can prove useful | SarcoidosisFavre-Racouchot syndromeTrichoepitheliomaSyringomaSebaceous hyperplasia | Acrokeratoelastoidosis (rare variant of palmoplantar keratoderma that may occur sporadically or as autosomal dominant genodermatosis)Actinic elastosis |
| Treatment | ElectrodesiccationCurettageCryotherapyIntralesional corticosteroidsDermabrasionCO2 and YAG laser | Topical retinoidsSystemic ascorbic acidDermabrasionChemical peelingCryotherapyPhototherapyCO2 and YAG laser |
Abbreviations: PAS, periodic acid–Schiff; YAG, yttrium aluminum garnet.
In the case we present, the diagnosis was confirmed by the correlation between clinical and histopathologic findings, which is supported to a large extent by immunohistochemistry. The clinical distribution of the lesions, which was similar to that described previously, enabled us to distinguish the condition from colloid milium.3 Nodular amyloidosis was ruled out through the absence of amyloid deposit, which in the present case was confirmed by inconclusive crystal violet staining and negative immunohistochemistry findings.
The diagnosis of degenerative collagenous and elastotic plaques of the hands is supported by its limitation to the hands and elastic fiber abnormalities in histopathology. However, as elastic fiber abnormalities are also reported in colloid milium, we might consider whether the latter is a clinical type of the former.
FundingThe authors declare that no funding was received for this publication.
Conflicts of InterestThe authors declare that they have no conflicts of interest.