A 2-year-old girl presented with a 3-month history of asymptomatic annular erythematous skin eruptions. Each plaque began as a small erythematous papule that enlarged, acquiring an annular configuration with central clearing. During this time some lesions spontaneously disappeared, leaving hyperpigmentation. The patient did not present constitutional symptoms. At the age of 1, she had been diagnosed with Disseminated Juvenile Xantogranuloma, without neurologic, ophthalmologic or other visceral involvement. She was otherwise healthy, had neither allergies nor a significant family history. There was no history of insect bites or exposure to animals and she had not received any medications previous to the eruption.
Physical examination revealed multiple annular and polycyclic erythematous plaques, with indurated borders and petechiae on the rims. The plaques were devoid of vesicles, crusts, erosions or desquamation (Fig. 1) and were distributed on her upper chest, abdomen and upper back. There was no hepatosplenomegaly, lymphadenopathy, or arthritis.
Laboratory studies disclosed a normal white cell count with normal differential. Immunoglobulin G titers were slightly elevated; IgM, IgA, IgE, antistreptolysin O titers; serum levels of C3 and C4 were normal. Anti-SS-A (Ro) and anti-SS-B (La) antibodies were negative. A stool examination for parasites and serologic tests for Toxocara, Bartonella hensenlae, Epstein–Barr virus and hepatitis B virus infection were negative.
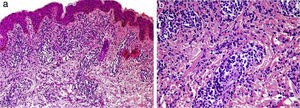
Histological examination of an annular plaque revealed superficial and deep perivascular and interstitial mixed-cell dermatitis. The deep dermal infiltrate was composed predominantly of neutrophils with abundant nuclear dust. Other vasculitis signs were absent (Fig. 2). Clinical and histopathological features were consistent with Neutrophilic Figurate Erythema of Infancy (NFEI).
Histological examination of a biopsy specimen taken from an indurated border of one plaque, hematoxylin–eosin stain (a) superficial and deep perivascular and interstitial infiltrate, without epidermal changes (Hematoxilina-Eosina 80X). (b) The deep dermal infiltrate was composed predominantly of neutrophils, with abundant nuclear dust, without other signs of vasculitis (Hematoxilina-Eosina 100X).
Two months after the consultation, the patient presented clinical and laboratory findings suggestive of mononucleosis syndrome due to Epstein–Barr virus. During the infection, the lesions increased in size and number. No improvement was seen during febrile periods.
Ten months after the beginning of plaques, a complete blood count was performed, which showed leukocytosis: 28,600WBC/mm3 with 22% monocytes and blast cells. A myelogram showed hypercellularity and 12% blast cells with monocyte-like appearance. The immunophenotype showed 17% immature monocytoid cells. Her fetal hemoglobin concentration was 24%. The translocation study (t9:22, t8:1 and t15:17) was negative. Therefore, juvenile myelomonocytic leukemia (JMML) was diagnosed. She began oral chemotherapy with hydroxiurea, observing an important improvement in the cutaneous lesions.
DiscussionAnnular or figurate erythemas of infancy (AEI) are characterized by a primary annular, circinate, arcuate or polycyclic pattern of cutaneous lesions.1,2 The lesions may be due to a known cause (rheumatic marginated erythema, neonatal lupus, erythema chronicum migrans) or may be idiopathic3 and may present with a localized or broad distribution.2,3
NFEI belongs to those figurate erythemas of unknown etiology.3 It is characterized by papular erythematous eruptions with rapid centrifugal enlargement to annular or polycyclic asymptomatic plaques with indurated borders devoid of vesicles, crusts or desquamation.4,5 Frequently, the eruptions begin on the face and then spread centrifugally to the limbs. The patches tend to disappear within 2–4 weeks, but the disease course is chronic.1,3
Histologically, NFEI is characterized by a superficial and deep, perivascular and interstitial infiltrate of neutrophils associated with leukocytoclasis but without other signs of vasculitis.1,2,4,5
Differential diagnosis of NFEI includes annular erythemas of infancy and dermatoses with a prominent neutrophilic infiltrate such as Sweet syndrome (SS) and pyoderma gangrenosum, urticarial lesions of dermatitis herpetiformis or linear IgA dermatosis, early lesions of bullous lupus erythematosus, Still disease, Sjögren's syndrome and early leukocytoclastic vasculitis.2
Sweet syndrome (SS) was very important in our differential diagnosis, considering the association with JMML presented in this case. However, our patient lacked typical manifestations of SS, as the lesions were asymptomatic and neither fever nor neutrophilia were present.2 Furthermore, paraneoplastic SS in children usually presents mucosal involvement, anemia and thrombocytopenia, and the neoplasm is concomitant with skin eruptions.7,8 Finally, SS histological findings differ from NFEI, as SS is characterized by a dense nodular or diffuse dermal infiltrate of neutrophils with nuclear dust with a variable amount of lymphocytes, histocytes, extravasated erythrocytes and a Grenz zone,2,7,8 findings not found in NFEI descriptions or in this patient.
Some authors have described cases of recurrent annular neutrophilic dermatosis in adulthood9 and have included this condition in the spectrum of neutrophilic dermatoses.
Although NFEI has been considered a benign chronic condition, only three pediatric cases have been reported.2,4,6 The association with a hematological neoplasm and its response to its treatment in our patient suggest that NFEI may be among the group of neutrophilic dermatoses. Cytokines and other biochemical mediators produced by blast cells could be involved in the development or maintenance of the skin lesions.
A standard treatment for NFEI has not been established. Previous reported treatments include topical steroids, systemic corticosteroids, hydroxychloroquine and colchicine, with poor responses.1,5
We present the first case of NFEI associated with JMML. Histological findings and the association with a hematological neoplasm suggest that NFEI may be in the spectrum of neutrophilic dermatoses. Therefore, after a diagnosis of NFEI an exhaustive study to exclude inflammatory diseases and neoplasms is warranted.