The Psoriasis Area Severity Index (PASI) is the most widely used scale for assessing the severity of psoriasis and for therapeutic decision making. On the basis of the PASI score, patients have been stratified into 2 groups: mild disease and moderate-to-severe disease.
ObjectiveTo draft a proposal for the definition and characterization of moderate psoriasis based on PASI and Dermatology Life Quality Index (DLQI) scores.
Material and methodsA group of 6 dermatologists with experience in the treatment of psoriasis undertook a critical review of the literature and a discussion of cases to draft a proposal.
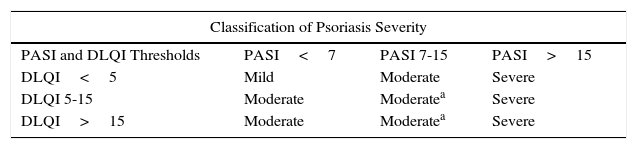
ResultsIn order of priority, PASI, DLQI, and body surface area (BSA) are the parameters to be used in daily practice to classify psoriasis as mild, moderate, or severe. Severity should be assessed on the basis of a combined evaluation and interpretation of the PASI and DLQI. And 3, PASI and DLQI should carry equal weight in the determination of disease severity. On this basis, psoriasis severity was defined using the following criteria: mild, PASI<7 and DLQI<7; moderate, PASI=7-15 and DLQI=5-15 (classified as severe when difficult-to-treat sites are affected or when there is a significant psychosocial impact); severe, PASI >15, independently of the DLQI score.
ConclusionsA more precise classification of psoriasis according to disease severity will improve the risk-benefit assessment essential to therapeutic decision making in these patients.
El Psoriasis Area Severity Index (PASI) es la escala de medida más utilizada para la valoración de la gravedad de la psoriasis y la toma de decisión para la indicación de tratamiento. Atendiendo a su valor se han diferenciado 2 grupos de pacientes: psoriasis leve y moderada-grave.
ObjetivoElaborar una propuesta para la definición y caracterización de la psoriasis moderada mediante el PASI y el DLQI.
Material y métodosUn grupo de 6 dermatólogos con experiencia en tratar psoriasis planteó la revisión crítica de la literatura y discusión de casos clínicos para elaborar una propuesta.
Resultados1) PASI, DLQI y BSA son, en orden de prioridad, los parámetros a emplear en la práctica clínica para la clasificación de la psoriasis leve, moderada y grave; 2) la evaluación de la gravedad debe incluir la evaluación e interpretación conjunta del PASI y del DLQI; y 3) la evaluación del PASI y del DLQI debería tener igual relevancia a la hora de determinar la gravedad de la psoriasis. Conforme a esto, se definieron los siguientes criterios de caracterización de psoriasis: a) leve: PASI<7 y DLQI<7; b) moderada: PASI 7-15 y DLQI 5-15 (grave en caso de localizaciones de difícil acceso para tratamientos o que supongan impacto psicosocial importante); y c) grave: PASI>15, independientemente de la puntuación DLQI.
ConclusionesUna mejor caracterización de los pacientes en función de su gravedad permitirá una mejora del balance de riesgos y beneficios en el que se fundamente la toma de decisiones terapéuticas.
Therapeutic decision making in patients with psoriasis is based on assessment of the severity of the disease, its impact on the patients’ quality of life, and the presence of comorbid conditions (mainly psoriatic arthritis, metabolic disorders, and cardiovascular risk). Currently, the psoriasis area severity index (PASI), body surface area (BSA), and Dermatology Life Quality Index (DLQI) are still considered by clinical guidelines as the most appropriate instruments for assessing the severity of cutaneous disease and its impact on quality of life. The guidelines stratify the severity of psoriasis into 2 large groups in accordance with the intensity of symptoms: mild psoriasis and moderate to severe psoriasis. The need or indication for systemic treatment and phototherapy is limited to those patients with moderate to severe psoriasis, whereas those patients with mild psoriasis are candidates for topical treatment. The correct classification of severity is, therefore, critical for therapeutic decision making.1–3
This classification, however, faces 2 important limitations. First, there is no absolute consensus on the thresholds for PASI and DLQI to provide a clinically coherent differentiation between mild and moderate to severe psoriasis.4 Most clinical trials of biologic agents for psoriasis define moderate to severe psoriasis as PASI or BSA greater than 10 or 10%, respectively, and DLQI greater than 10.5,6 However, the fact that assignment of patients with more severe disease to a moderate to severe group implies the same therapeutic approach for a highly heterogenous group of patients, whose PASI could range from 10 to a maximum of 72.5 Thus, the consensus document of the Academia Española de Dermatología y Venereología, published in 2009 by Puig et al,3 already questioned whether PASI and BSA might be inadequate means for appropriately defining severity and whether factors such as site or special clinical forms should be taken into account if associated with greater psychological or social impact for the patients. The update to the consensus document, published in 2016, also considered a combined definition of moderate to severe psoriasis as PASI>10, BSA>10%, and DLQI>10, clarifying that it is not essential to use quality of life indices to include a patient in this category.7
The availability of increasingly effective treatments for psoriasis in turn demands an improved definition of severity of cutaneous and joint involvement and its impact on the patients’ quality of life. A more precise definition of the severity of psoriasis, especially in terms of better differentiation between moderate psoriasis and severe psoriasis would enable better matching of treatment burden to disease severity and the extracutaneous repercussions. The objective of this study was to propose a definition for classification of moderate psoriasis through revision of the PASI, BSA, and DLQI thresholds.
MethodIn a preliminary phase, a working group was selected comprising 6 dermatologists each with at least 9 years experience in the treatment of psoriasis from 4 different autonomous communities in Spain (Madrid, Valencia, Andalusia, and Catalonia). A 3-phase process was then followed: 1) literature review; 2) elaboration of a questionnaire with relevant questions to help guide the proposal; and 3) face-to-face meeting with critical review of the selected scientific evidence, completion of the questionnaire and discussion of its content, discussion of preselected clinical cases, and drafting of the proposal.
The literature search was performed by an independent scientific consultancy following a search strategy with terms pertaining to psoriasis along with different parameters used for assessing severity and quality of life and terms pertaining to diagnosis, prognosis, prevalence, incidence, therapeutic guidelines, and consensuses. The search strategy was restricted to studies performed in humans, excluding clinical trials, published from 2005 until present in Spanish or English, and also included therapeutic guidelines, consensus documents, and assessment reports at a regional or hospital level. The searches were performed using the OVID platform in the MEDLINE, Embase, and Cochrane databases.
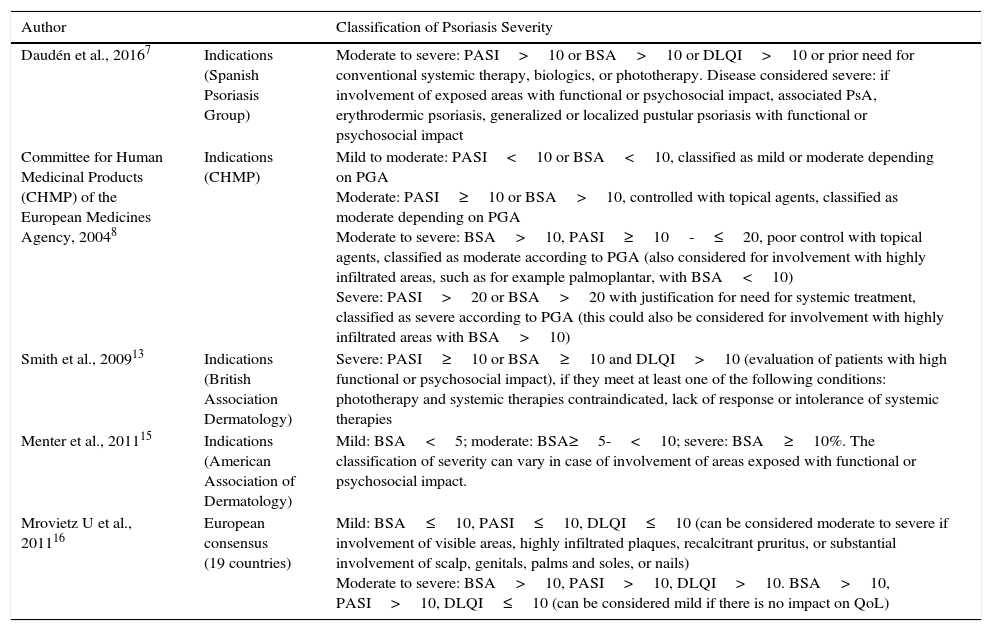
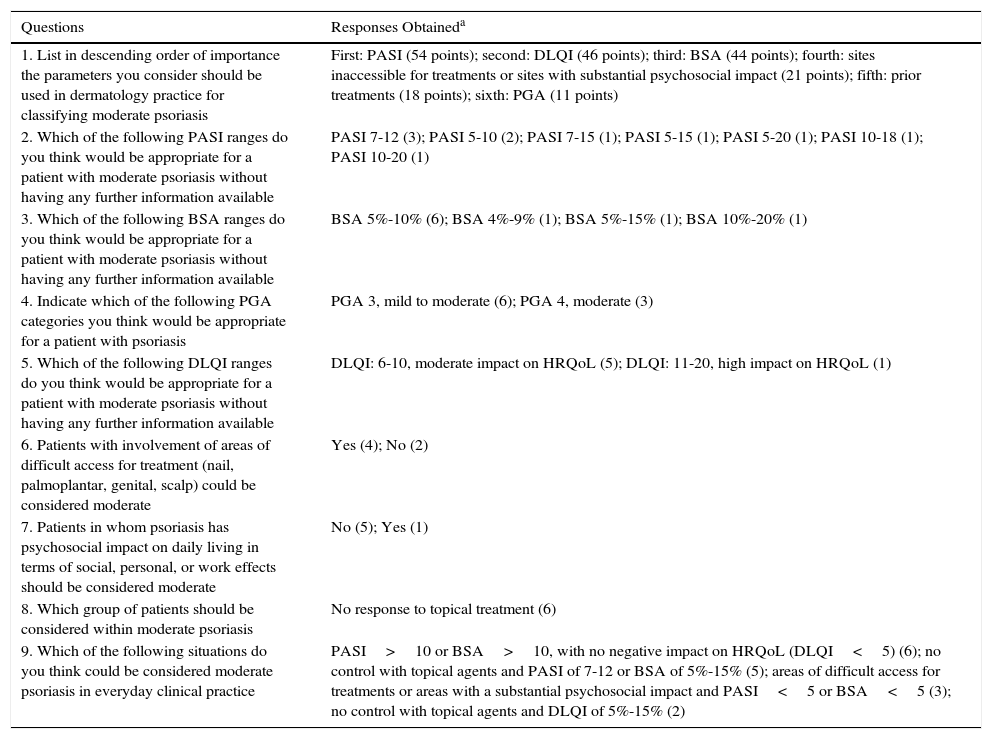
Using the evidence identified (Table 1), a questionnaire was drawn up that included a battery of 9 questions to be subsequently answered by the group of participating experts (Table 2). In the face-to-face phase, the evidence identified was presented and debated, and the participants filled out the questionnaire, and the extent of agreement for each question was then assessed and a proposal was then drawn up for characterization of mild, moderate, and severe psoriasis.
Criteria for Classification of Psoriasis (Scientific Societies and European Consensus).
| Author | Classification of Psoriasis Severity | |
|---|---|---|
| Daudén et al., 20167 | Indications (Spanish Psoriasis Group) | Moderate to severe: PASI>10 or BSA>10 or DLQI>10 or prior need for conventional systemic therapy, biologics, or phototherapy. Disease considered severe: if involvement of exposed areas with functional or psychosocial impact, associated PsA, erythrodermic psoriasis, generalized or localized pustular psoriasis with functional or psychosocial impact |
| Committee for Human Medicinal Products (CHMP) of the European Medicines Agency, 20048 | Indications (CHMP) | Mild to moderate: PASI<10 or BSA<10, classified as mild or moderate depending on PGA Moderate: PASI≥10 or BSA>10, controlled with topical agents, classified as moderate depending on PGA Moderate to severe: BSA>10, PASI≥10-≤20, poor control with topical agents, classified as moderate according to PGA (also considered for involvement with highly infiltrated areas, such as for example palmoplantar, with BSA<10) Severe: PASI>20 or BSA>20 with justification for need for systemic treatment, classified as severe according to PGA (this could also be considered for involvement with highly infiltrated areas with BSA>10) |
| Smith et al., 200913 | Indications (British Association Dermatology) | Severe: PASI≥10 or BSA≥10 and DLQI>10 (evaluation of patients with high functional or psychosocial impact), if they meet at least one of the following conditions: phototherapy and systemic therapies contraindicated, lack of response or intolerance of systemic therapies |
| Menter et al., 201115 | Indications (American Association of Dermatology) | Mild: BSA<5; moderate: BSA≥5-<10; severe: BSA≥10%. The classification of severity can vary in case of involvement of areas exposed with functional or psychosocial impact. |
| Mrovietz U et al., 201116 | European consensus (19 countries) | Mild: BSA≤10, PASI≤10, DLQI≤10 (can be considered moderate to severe if involvement of visible areas, highly infiltrated plaques, recalcitrant pruritus, or substantial involvement of scalp, genitals, palms and soles, or nails) Moderate to severe: BSA>10, PASI>10, DLQI>10. BSA>10, PASI>10, DLQI≤10 (can be considered mild if there is no impact on QoL) |
Abbreviations: BSA, body surface area; DLQI, dermatology life quality index; PASI, psoriasis area suface index; PGA, physician global assessment.
Responses to the Questions Included in the Questionnaire.
| Questions | Responses Obtaineda |
|---|---|
| 1. List in descending order of importance the parameters you consider should be used in dermatology practice for classifying moderate psoriasis | First: PASI (54 points); second: DLQI (46 points); third: BSA (44 points); fourth: sites inaccessible for treatments or sites with substantial psychosocial impact (21 points); fifth: prior treatments (18 points); sixth: PGA (11 points) |
| 2. Which of the following PASI ranges do you think would be appropriate for a patient with moderate psoriasis without having any further information available | PASI 7-12 (3); PASI 5-10 (2); PASI 7-15 (1); PASI 5-15 (1); PASI 5-20 (1); PASI 10-18 (1); PASI 10-20 (1) |
| 3. Which of the following BSA ranges do you think would be appropriate for a patient with moderate psoriasis without having any further information available | BSA 5%-10% (6); BSA 4%-9% (1); BSA 5%-15% (1); BSA 10%-20% (1) |
| 4. Indicate which of the following PGA categories you think would be appropriate for a patient with psoriasis | PGA 3, mild to moderate (6); PGA 4, moderate (3) |
| 5. Which of the following DLQI ranges do you think would be appropriate for a patient with moderate psoriasis without having any further information available | DLQI: 6-10, moderate impact on HRQoL (5); DLQI: 11-20, high impact on HRQoL (1) |
| 6. Patients with involvement of areas of difficult access for treatment (nail, palmoplantar, genital, scalp) could be considered moderate | Yes (4); No (2) |
| 7. Patients in whom psoriasis has psychosocial impact on daily living in terms of social, personal, or work effects should be considered moderate | No (5); Yes (1) |
| 8. Which group of patients should be considered within moderate psoriasis | No response to topical treatment (6) |
| 9. Which of the following situations do you think could be considered moderate psoriasis in everyday clinical practice | PASI>10 or BSA>10, with no negative impact on HRQoL (DLQI<5) (6); no control with topical agents and PASI of 7-12 or BSA of 5%-15% (5); areas of difficult access for treatments or areas with a substantial psychosocial impact and PASI<5 or BSA<5 (3); no control with topical agents and DLQI of 5%-15% (2) |
Abbreviations: BSA, body surface area; DLQI, dermatology life quality index; HRQoL, health-related quality of life; PASI, psoriasis area severity index; PGA, physician global assessment.
Responses only shown if used at least once. For question 1, a value of 9 (most important) to 1 (least important) was assigned to each response item, and the values assigned to each parameter by the 6 participants were summed; for the remaining questions, from 2 to 9, the number of experts who chose each response option is shown.
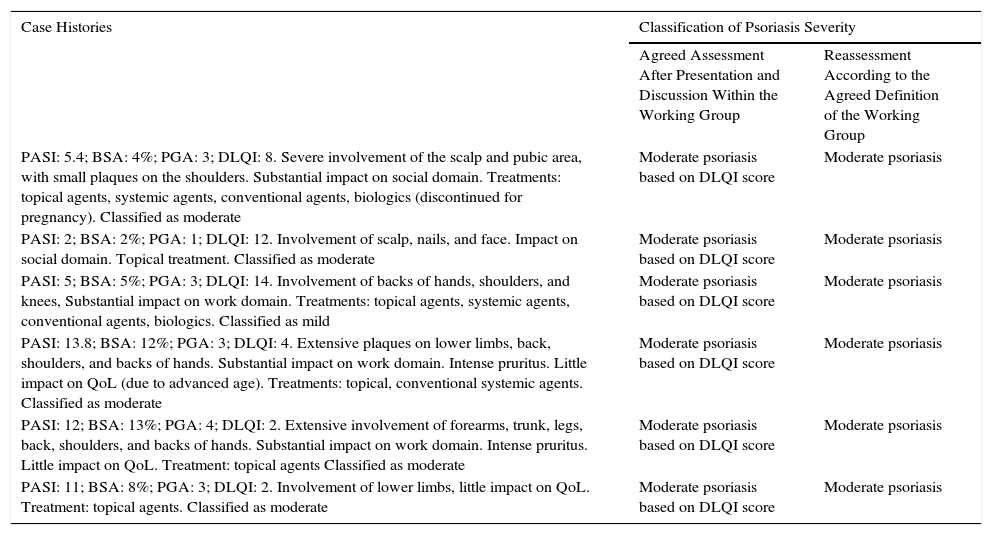
The participants presented clinical cases from their clinics which met the following pre-established criteria: 1) patient with PASI<10 and BSA<10%, and who would therefore be considered as having mild psoriasis according to the current guidelines, but given the site or impact on quality of life, could potentially be considered as having moderate psoriasis; and 2) patient with PASI>10 or BSA>10% and who would therefore be considered as having moderate to severe psoriasis according to the current guidelines, but given the site or impact on quality of life, could potentially be considered as having moderate psoriasis (Table 3). The clinical cases were finally reassessed according to the proposed classification.
Classification of the Selected Case Histories.
| Case Histories | Classification of Psoriasis Severity | |
|---|---|---|
| Agreed Assessment After Presentation and Discussion Within the Working Group | Reassessment According to the Agreed Definition of the Working Group | |
| PASI: 5.4; BSA: 4%; PGA: 3; DLQI: 8. Severe involvement of the scalp and pubic area, with small plaques on the shoulders. Substantial impact on social domain. Treatments: topical agents, systemic agents, conventional agents, biologics (discontinued for pregnancy). Classified as moderate | Moderate psoriasis based on DLQI score | Moderate psoriasis |
| PASI: 2; BSA: 2%; PGA: 1; DLQI: 12. Involvement of scalp, nails, and face. Impact on social domain. Topical treatment. Classified as moderate | Moderate psoriasis based on DLQI score | Moderate psoriasis |
| PASI: 5; BSA: 5%; PGA: 3; DLQI: 14. Involvement of backs of hands, shoulders, and knees, Substantial impact on work domain. Treatments: topical agents, systemic agents, conventional agents, biologics. Classified as mild | Moderate psoriasis based on DLQI score | Moderate psoriasis |
| PASI: 13.8; BSA: 12%; PGA: 3; DLQI: 4. Extensive plaques on lower limbs, back, shoulders, and backs of hands. Substantial impact on work domain. Intense pruritus. Little impact on QoL (due to advanced age). Treatments: topical, conventional systemic agents. Classified as moderate | Moderate psoriasis based on DLQI score | Moderate psoriasis |
| PASI: 12; BSA: 13%; PGA: 4; DLQI: 2. Extensive involvement of forearms, trunk, legs, back, shoulders, and backs of hands. Substantial impact on work domain. Intense pruritus. Little impact on QoL. Treatment: topical agents Classified as moderate | Moderate psoriasis based on DLQI score | Moderate psoriasis |
| PASI: 11; BSA: 8%; PGA: 3; DLQI: 2. Involvement of lower limbs, little impact on QoL. Treatment: topical agents. Classified as moderate | Moderate psoriasis based on DLQI score | Moderate psoriasis |
Abbreviations: BSA, body surface area; DLQI, dermatology life quality index; PASI, psoriasis area surface index; PGA, physician global assessment; QoL, quality of life.
The literature review identified 14 citations that included definitions of different categories of severity of psoriasis.7–20Table 1 summarizes the definitions of psoriasis severity categories according to the main scientific societies and the European consensus that included the opinion of psoriasis experts in 19 countries.7,8,13,15,16 After review and discussion of the available scientific evidence, completion of the questionnaire, and assessment of the clinical cases presented, the working group considered the following proposals:
- 1.
PASI, DLQI, and BSA are, in order of priority and in accordance with the available evidence, the parameters to use in clinical practice for classification of mild, moderate, and severe psoriasis.
- 2.
Assessment of the severity of psoriasis should include joint assessment and interpretation of PASI and DLQI scores. Assessment of the PASI and DLQI should have the same importance for determining the severity of psoriasis, because they support the assessment made by the dermatologist and are consistent with the patients’ perception.
- 3.
The PASI range 7-15 could be considered appropriate for defining moderate psoriasis.
- 4.
The DLQI range 6-10 could be considered appropriate for defining moderate psoriasis.
- 5.
The BSA range 5%-10% could be considered appropriate for defining moderate psoriasis.
- 6.
The presence of nail, palmoplantar, genital, and scalp involvement could be considered moderate psoriasis due to the impact on the functional capacity of the patient when these sites are involved. However, it was considered that involvement of certain difficult-to-treat sites could be appropriately assessed with the DLQI, and so it would not be necessary to include these sites in the definition of moderate or severe psoriasis.
- 7.
The definition of mild, moderate, and severe psoriasis could be based on the combination of ranges for PASI and DLQI described (Table 4).
Table 4.Proposed Classification and Definition of Mild, Moderate to Severe, and Severe Psoriasis According to PASI and DLQI Thresholds.
Classification of Psoriasis Severity PASI and DLQI Thresholds PASI<7 PASI 7-15 PASI>15 DLQI<5 Mild Moderate Severe DLQI 5-15 Moderate Moderatea Severe DLQI>15 Moderate Moderatea Severe Abbreviations: DLQI, dermatology life quality index; PASI, psoriasis area severity index.
Table 2 summarizes the responses for the questions included in the questionnaire, and Table 3 summarizes the outcome of the reassessment of clinical cases presented in the meeting in accordance with the definitions of the consensus.
DiscussionReview of the retrieved literature highlighted the variability in terms of thresholds for PASI, BSA, and DLQI used in different studies for defining moderate and moderate to severe psoriasis (Table 1).7–20 Likewise, the discussion of clinical cases presented also highlighted difficulties for reaching consensus agreements among experts, particularly for the classification of moderate psoriasis in patients with high PASI or BSA, whereas the consensus was absolute for those patients with lower PASI or BSA, regardless of the impact on DLQI. This discrepancy might indicate that clinicians continue to give more weight to objective assessments (PASI, BSA) than subjective patient-reported assessments (DLQI).
With regards the proposed definition of mild, moderate, and severe psoriasis, 2 points are worth highlighting. First, the areas of uncertainty or limitations of the psoriasis severity classification have been reduced to a single scenario with 9 possible options. Second, the integrated application of objective assessment by the physician (PASI) and the patient perception (DLQI) is proposed. This integration is particularly useful for the definition of moderate psoriasis. Thus, any patients with an impact on the quality of life indicated by a DLQI greater than 15 should be considered as moderate or severe psoriasis, regardless of the objective assessment of the dermatologist (PASI); in other words, a patient with DLQI>15 could not be classified as having mild disease under any circumstances, regardless of the PASI score. Likewise, any patient with a PASI greater than 15 would be classified as having severe psoriasis, regardless of the impact of the disease on quality of life, and no patient with PASI less than 7 would be classified as having severe psoriasis, regardless of the impact on quality of life (Table 1).
The more appropriate characterization of patients with psoriasis according to their severity can better address needs that so far have not been met. First, it would homogenize groups of patients included in clinical trials. Second, the benefit risk assessment (efficacy versus toxicity and costs) that form the basis for therapeutic decisions could be adapted more exactly to the real needs of the patient, thereby avoiding possible overtreatment or undertreatment.
Another methodological limitation of the present study to take into account is that fact that a limited number of dermatologists participated (n=6), and so the conclusions reached cannot be considered as robust as a consensus document. Nevertheless, we believe that the proposed definition and classification of moderate and severe psoriasis agreed by this working group, which included experts in the management of psoriasis, may serve as a starting point for debate in a representative group of experts following an appropriate method (for example the Delphi method or similar). Such a consensus could be used and implemented in everyday clinical practice, and would without doubt lead to improved treatment of patients with psoriasis in Spain.
Ethical ResponsibilitiesProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed their hospital's protocol on the publication of data concerning patients.
Right to privacy and informed consentThe authors declare that patient data do not appear in this article.
FundingFor the present study, Celgene collaborated in the organization of meetings and the literature search performed by the independent scientific consultancy. Nobody associated with Celgene participated in drafting the proposals or had input in other content produced by this working group or in drafting the manuscript.
Conflicts of InterestMar Llamas-Velasco has participated in clinical trials, research projects, and training and consulting activities with the following companies: Abbvie, Celgene, Galderma, Janssen, Leo-Pharma, Lilly, Novartis, and Pfizer.
Pablo de la Cueva has participated as consultant and/or investigator and/or speaker for Abbvie, Almirall, Biogen, Boehringer, Celgene, Janssen, Leo-Pharma, Lilly, MSD, Novartis, Pfizer, and UCB.
Jaume Notario Rosa has received honoraria for consulting and training activities from Abbvie, Celgene, Janssen, Leo-Pharma, Lilly, MSD, Novartis, and Pfizer. He has participated in clinical trials and research projects sponsored by Abbvie, Janssen, MSD, Novartis, and Pfizer.
Leandro Martínez-Pilar has participated in research projects, and training and consulting activites with the following companies: Abbvie, Celgene, Janssen, Leo-Pharma, MSD, Novartis, and Pfizer.
Antonio Martorell has participated in training and consulting activities with the following companies: Abbvie, Celgene, Janssen, Isdin, MSD, Novartis, and Pfizer.
David Moreno-Ramírez has participated in research projects, and training and consulting activities with the following companies: Abbvie, Celgene, Janssen, Leo-Pharma, Lilly, MSD, Novartis, and Pfizer.
Please cite this article as: Llamas-Velasco M, de la Cueva P, Notario J, Martínez-Pilar L, Martorell A, Moreno-Ramírez D. Psoriasis moderada. Propuesta de definición. Actas Dermosifiliogr. 2017;108:911–917.