CLAPO syndrome (Capillary vascular malformation of the lower lip, Lymphatic malformations of the head and neck, Asymmetry and Partial/generalized Overgrowth) is a recently described entity, with very few published cases in the literature, and no standardized treatment. The objective of our study was to assess the efficacy and safety of PDL in patients with this syndrome. Seven patients were treated with two to four sessions of PDL at 595-nm wavelength. Laser therapy was performed using a spot size of 7 to 10mm, a pulse duration of 0.5–1.5ms and a fluence from 6 to 8J/cm2. Clinical photographs were taken before treatment and 3 weeks after procedure. Clearance of the erythema was >75% in 4 patients. Transient purpura was present in all patients for about 2 weeks and 1 patient presented post inflammatory hypopigmentation. In conclusion we consider that PDL seems to be a safe and effective treatment for capillary malformations of the CLAPO syndrome. A marked reduction in erythema was achieved in all patients with a low incidence of side effects.
El síndrome Capillary vascular malformation of the lower lip, Lymphatic malformations of the head and neck, Asymmetry and Partial/generalized Overgrowth (CLAPO) es una entidad recientemente descrita, con muy pocos casos publicados en la literatura, y sin tratamiento estandarizado. El objetivo de nuestro estudio fue evaluar la eficacia y seguridad del láser de colorante pulsado (PDL) en los pacientes con este síndrome. Tratamos a siete pacientes con dos a cuatro sesiones de PDL a longitud de onda de 595nm. La terapia láser fue realizada utilizando un tamaño de spot de 7 a 10mm, una duración del pulso de 0,5 a 1,5ms, y una fluencia de 6 a 8J/cm2. Se realizaron fotografías clínicas antes del tratamiento y tres semanas tras el procedimiento. La supresión del eritema fue >75% en cuatro pacientes. La púrpura transitoria estuvo presente en todos los pacientes durante alrededor de dos semanas, presentando un paciente con hipopigmentación postinflamatoria. A modo de conclusión consideramos que el PDL parece ser un tratamiento seguro y efectivo para las malformaciones capilares propias del síndrome CLAPO. Se logró una notable reducción del eritema en todos los pacientes, con baja incidencia de efectos secundarios.
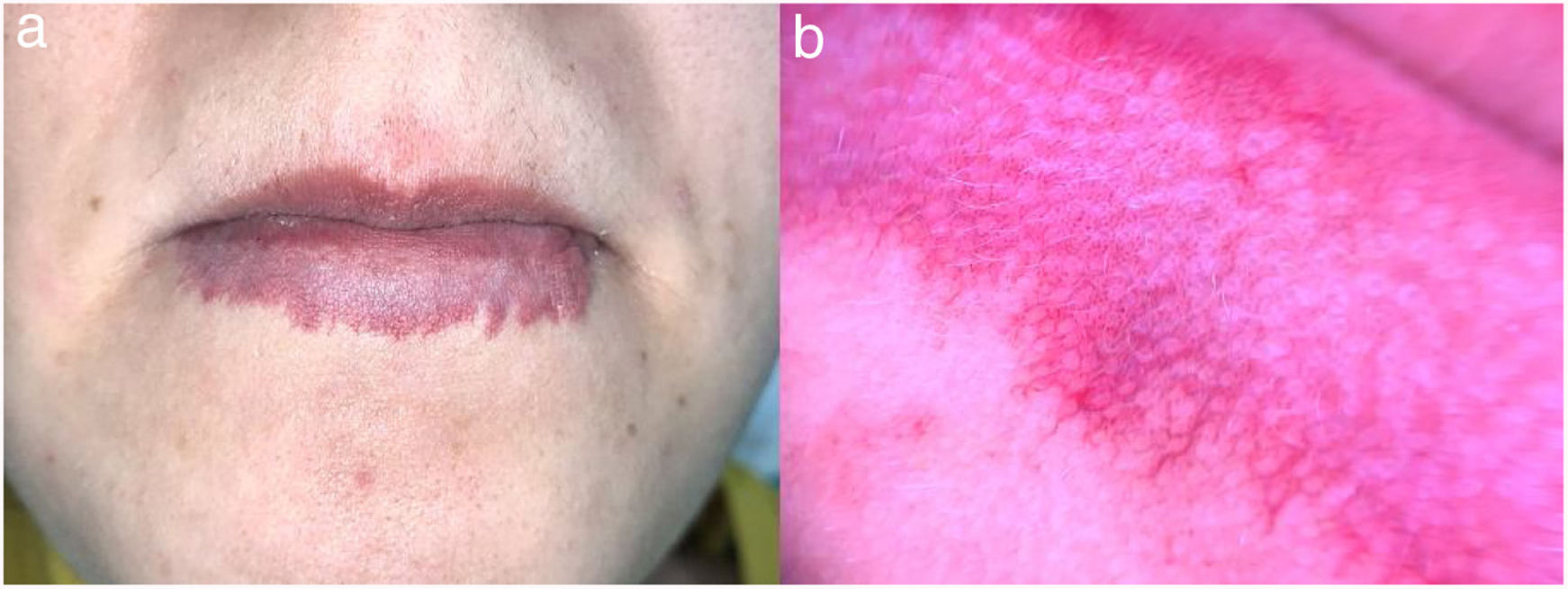
CLAPO syndrome is a rare vascular disorder described by López-Gutiérrez and Lapunzina in 2008, characterized by lower lip capillary malformation, lymphatic malformation, asymmetry of the face and limbs and partial/generalized overgrowth.1 Preliminary studies have demonstrated mosaic activating mutations in PIK3CA which may contribute to its variable clinical expressions.2 However, despite its heterogeneous phenotypic spectrum, capillary malformation of the lower lip seems to be a constant feature1,3 and is almost pathognomonic for this syndrome. This is usually a midline, symmetric, erythematous patch, present at birth and that may progressively expand beyond the vermilion (Fig. 1). In addition, capillary malformations might also affect other locations of the face including the forehead, lower cheek, mandible and chin.
The authors report a series of seven cases, wishing to discuss the efficacy and safety of 595-nm PDL for the treatment of CLAPO's capillary malformation.
Material and methodsSeven patients with a clinical diagnosis of CLAPO syndrome were enrolled in this study at the Dermatology Department of the Hospital Universitario Ramon y Cajal, Madrid, Spain. The group of patients was composed of 6 women and 1 man, ranging in age from 18 to 58 years old. All had a symmetric, sharply defined erythematous-violaceous patch of the lower lip, consistent with a capillary malformation. Additional clinical findings are summarized in Table 1. Patients were given detailed information prior to the first treatment, including the risks, benefits, potential complications and alternative treatments. Written informed consent was obtained to participate.
Patients were treated with 595-nm PDL irradiation (Cynergy, Cynosure, Massachusetts, USA) using a spot size of 7–10mm, a pulse duration from 0.5 to 1.5ms and fluence from 6 to 8J/cm2. Continuous airflow cooling was set at level 3 (Cryo5, Zimmer Medizinsysteme GmbH, Neu-Ulm, Germany) and the lesions were covered by a thin layer of ultrasound gel for epidermal protection. Intense purpura was intentionally produced in all cases; this occasionally required double passing, but pulse stacking was avoided. Treatments were repeated approximately every 2 months, up to four sessions.
Clinical improvement was assessed by comparing digital photographs of each patient taken at baseline and 3 weeks after the end of therapy.
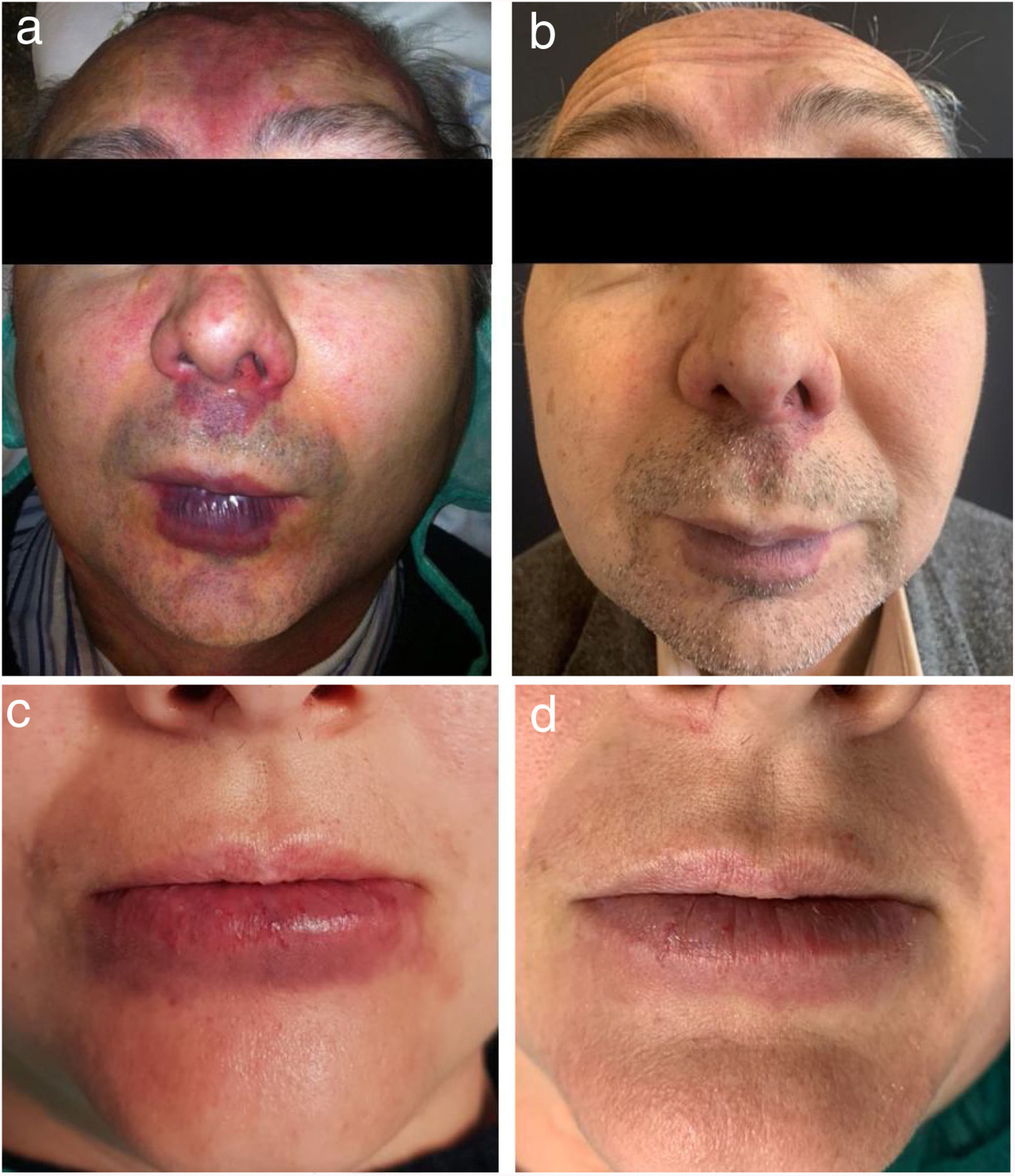
ResultsResults are shown in Table 1. All lesions responded to treatment, and a clearance of erythema superior to 75% was obtained in four patients. Treatment was well tolerated with no need for anesthesia or analgesia. Side effects included transient purpura for about 2 weeks, which was present in all patients and post-inflammatory hypopigmentation in one case (Fig. 2).
Patients and outcome.
| ID | Sex/age | Skin type | CM | LM | VM | Overgrowth | Nr sessions | Clearance erythema (%) |
|---|---|---|---|---|---|---|---|---|
| 1 | F/18 | II | Lower lip and adjacent skin | Tongue and lower lip | – | – | 2 | 75% |
| 2 | F/20 | III | Lower lip and adjacent skin | Intraoral pat of the lip | – | – | 2 | 75% |
| 3 | F/58 | II | Lower lip and adjacent skin | – | Mandibular region and neck | – | 2 | 50% |
| 4 | F/22 | III | Lower lip and adjacent skin | Chin, tongue and intraoral part of the lip | – | Partial. Left side of the face and neck | 3 | 75% |
| 5 | M/51 | III | Lower lip and adjacent skin Forehead, dorsum nose and philtrum | Tongue | Tongue | – | 4 | 75% |
| 6 | F/37 | II | Lower lip and adjacent skin | Intraoral pat of the lip | – | – | 2 | 50% |
| 7 | F/32 | III | Lower lip and adjacent skin | – | – | – | 2 | 50% |
F, female; M, male; CM, capillary malformation; LM, Lymphatic malformation; VM, venous malformation.
Laser parameters: spot size 7-10mm, pulse duration 0,5-1,5ms, fluence 6- 8J/cm2.
Capillary malformations are the most common type of vascular malformations. However, capillary malformation of the lower lip is an infrequent finding and is almost invariably related to the spectrum of CLAPO syndrome. This sign is always present at birth and may appear years to decades before the remaining features. Therefore, physicians must be aware of the possibility of this syndrome and maintain follow-up during infancy and adolescence.4 In comparison with the anterior midline lesions of the upper lip, that are typical of macrocephaly capillary malformation syndrome,5,6 capillary malformations of the lower lip do not tend to regress and may slowly expand beyond the vermilion. Change in color can also be expected, observing a transformation from red to more violaceus tones.
Pulsed dye laser has been widely used in vascular lesions, such as haemangiomas,7 port wine stains,8 telangiectasias9 and other conditions that present with facial erythema. To the best of our knowledge, there is only one case reported of CLAPO syndrome treated with PDL. However, parameters were not defined, and no substantial improvement was observed.4
From our experience, an intense purpura is necessary to obtain a good clinical response. This can be achieved either by using high fluences (6–8J/cm2) or by several passes separated by a minute. Nevertheless, a minimum of 2 sessions is required for a significant reduction (>50%) of the erythematous component.
Severe inflammatory reaction, swelling, crusting and rarely ulceration can be seen after treatment with PDL, especially when it involves the mucosa. However, the administration of oral or intramuscular glucocorticoids is not usually needed.
This report suggests that PDL is an effective option for the treatment of CLAPO's capillary malformations, since a marked reduction in erythema was achieved in all patients. Likewise, a good tolerance to treatment and a low incidence of serious side effects make it a very safe therapy and a first-line option in controlling the disease.
FundingThis work has not received any funding.
Conflict of interestThe authors declare that they have no conflict of interest.