Oral submucous fibrosis (OSMF) is a chronic, insidious, premalignant condition characterized by inflammation and progressive fibrosis of the oral mucosa that results in narrowing of the oral opening. It is strongly associated with areca nut chewing, a frequent habit in Southeastern Asia. Reports of OSMF in the European continent have been exceptional to date. However, due to immigration from endemic areas, an increasing incidence of this disease is expected. We report a recently diagnosed case at our department.
A 60-year-old woman, a native of Bangladesh, presented with a 24-month history of progressive limitation in mouth opening and oral pain during food intake. Her past medical history was unremarkable.
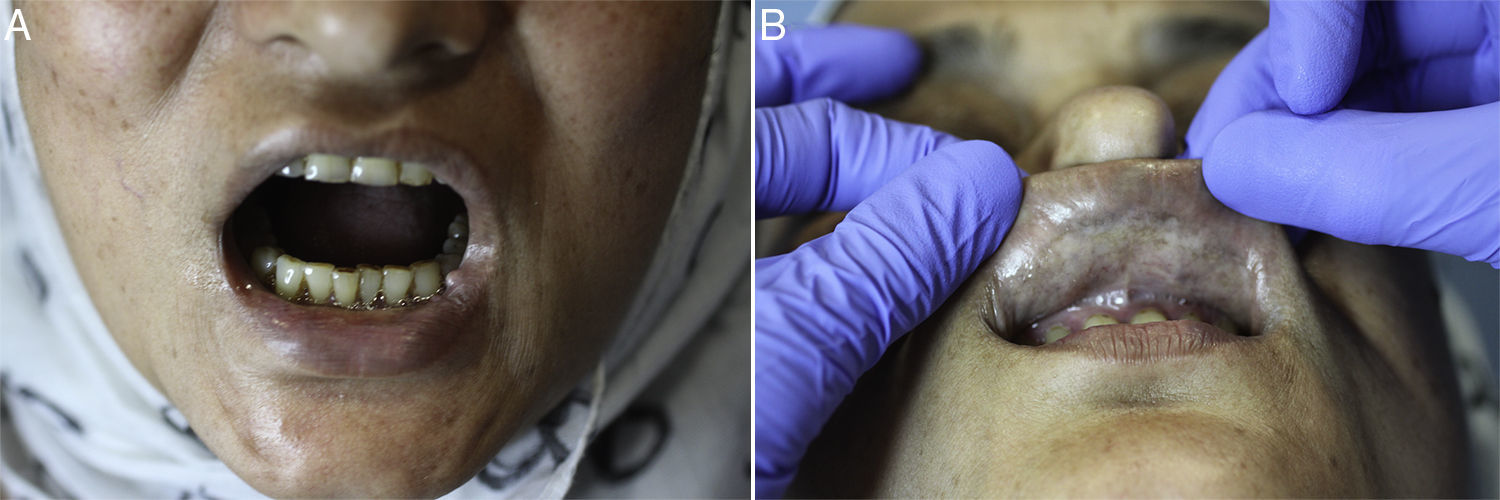
Physical examination revealed a diffuse paleness and hardening of the oral mucosa. Whitish reticular pigmentation of the alveolar and labial mucosa was also observed. The patient presented trismus, difficulty with tongue protrusion, and limited vertical mouth opening; the distance between the superior and inferior central incisor edges was 18mm (average, 40mm). On palpation, symmetrical fibrous bands in the oral mucosa were also noticed (Fig. 1). Blood tests revealed mild iron deficiency anemia and immunologic tests were negative for antinuclear antibodies. Hepatitis C and anti-HBc antigen tests were negative. A punch biopsy for histopathologic study was performed.
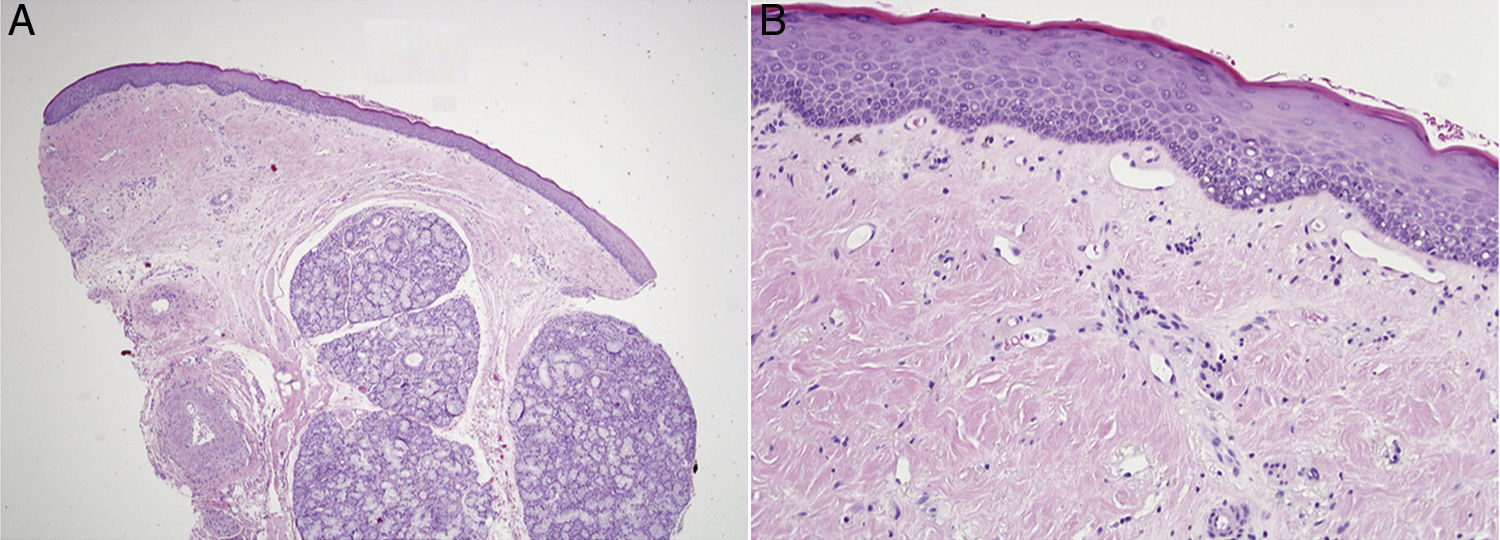
Hematoxylin and eosin sections showed a slightly hyperkeratotic atrophic mucosa and diffuse hyalinization of the subepithelial stroma. A discrete lymphoid interstitial inflammatory infiltrate with pigment incontinence was present in the upper submucosa. Concentric fibrotic layers surrounding mucous glands and blood vessels were also noted. A direct immunofluorescence study was negative (Fig. 2).
(A) Oral mucosa biopsy specimen showing hyalinization and fibrosis of the submucosa with a mild submucosal inflammatory infiltrate (hematoxylin–eosin, original magnification ×40). (B) Epithelial atrophy without dysplasia and mild hyperkeratosis. Scattered mononuclear cell infiltration and pigment incontinence in the submucosa (hematoxylin–eosin, original magnification ×200).
The findings were suggestive of OSMF. We asked the patient if she chewed areca nut and she admitted having done so many times a day for the past 20 years.
The patient was started on oral glucocorticoids (prednisone 0.5mg/kg/d for 3 weeks with progressive dose tapering and pentoxifylline 400mg, 3 times a day), and was strongly advised to stop chewing areca nuts. Subjective clinical improvement, with decreasing symptoms, was observed after 3 months.
OSMF is rare in Spain. The most common cause is the chewing of areca nuts, either alone or in association with other substances such as tobacco, spices, or lime wrapped in a betel leaf.1,2 Habitual long term chewing leads to nonreversible fibrosis of the oral mucosa.
The clinical manifestations usually appear within 2–5 years of starting the chewing habit. The most common clinical presentation is limited mouth opening, followed by a burning sensation. Pain or tongue protrusion difficulties may also be reported by some patients. Mucosal blanching and palpable fibrous bands are the most common findings in the physical examination. Others include shrunken uvula, depapillated tongue, and ulceration.3
Histopathological features include a combination of mucosal and submucosal changes. Atrophic changes such as thinning of the epithelium, liquefaction degeneration, and pigment incontinence are usually present. Dysplasia may be observed in up to 8.6% of cases.4 Submucosal findings are characterized by almost constant stromal fibrosis and hyalinization associated with a diffuse discrete chronic mononuclear inflammatory infiltrate. Patients with OSMF have an increased risk of squamous cell carcinoma, which may develop in about 2.3–7.6% of cases.5
The pathogenesis of OSMF has not been fully elucidated, although mechanisms such as arecoline hydrolysis have been postulated.
The differential diagnosis should include certain temporomandibular joint disorders (ankylosis), physical damage to the oral mucosa (induced, for example, by radiotherapy or caustic ingestion), autoimmune connective diseases leading to mucosal sclerotic changes (scleroderma), metabolic disorders (amyloidosis), and immunologically mediated mucocutaneous disorders (lichen planus or mucous membrane pemphigoid). A tissue sample may be indicated in cases of diagnostic doubt and investigations of dysplasia.
Cessation of areca chewing has been reported to stop progression and in rare cases, improve the condition, and should be recommended at all stages of disease.6
Several treatments have been proposed for OSMF, but in most cases, clear evidence of their effectiveness is lacking. Oral or intralesional corticosteroids are the most widely used treatment. Pentoxifylline, interferon gamma, and lycopene have been occasionally been used with variable results.7
Treatment seems to be useful only in the early stages of disease, before the development of trismus. In advanced stages, management approaches focus on early detection of oral cancer and surgical procedures to restore an acceptable degree of oral opening. Early recognition and diagnosis is therefore important. Long-term follow-up is advisable due to the risk of malignant transformation into squamous cell carcinoma.
Conflict of interestThe authors declare no conflict of interest.
We would like to thank the patient for providing her written consent and permission to publish this case report and the accompanying clinical pictures.