This is a rare case that presented with pyoderma gangrenosum-like cervical ulcers followed by painful subcutaneous nodules on the lower legs showing neutrophilic panniculitis on the histopathological examination in a patient with myelodysplastic syndrome.
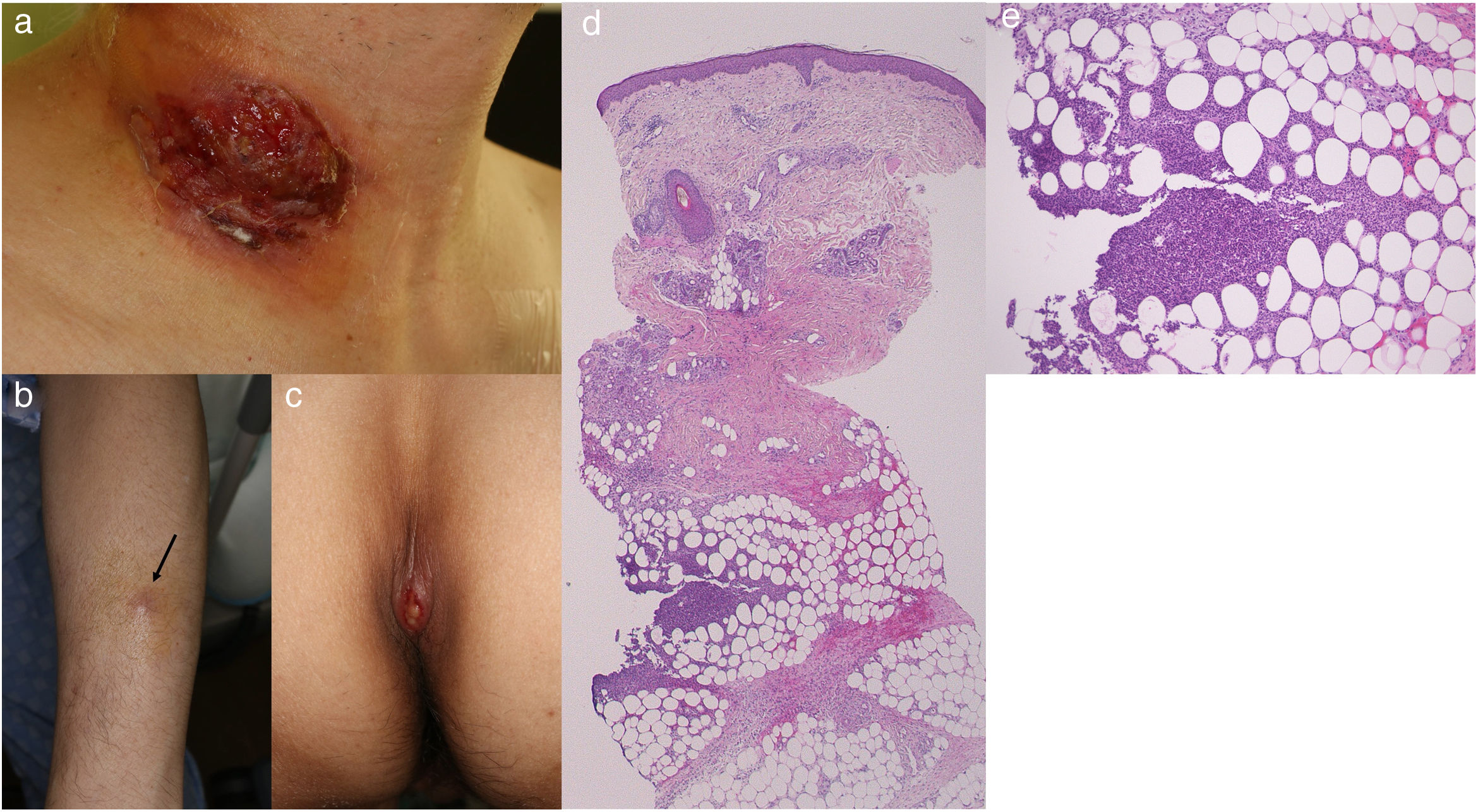
This is the case of a 51-year-old man hospitalized due to myelodysplastic syndrome who received chemotherapy with azacytidine without granulocyte colony-stimulating factor. He developed a skin ulcer and subcutaneous induration at the central venous catheter insertion site on the right neck (Fig. 1a). Although skin biopsy was not performed at this time, PG was suspected, and oral prednisolone (PSL) (60mg/day) was started. The skin ulcer healed in 3 weeks. After a remission induction therapy, anthracycline was administered for 3 days and cytarabine for 7, PSL was down-titrated to 25mg, and no recurrences of the cervical lesions were seen. However, new and painful subcutaneous indurations appeared on the extremities with high fever. The blood test showed elevated C-reactive protein levels (2.51mg/dL) and decreased platelet count (1.0×104/μL). The physical examination revealed the presence of multiple tender subcutaneous erythematous indurations (about 0.5–2cm in diameter), on the forearms and thighs, as well as sacral ulcer (Fig. 1b, c). Local samples for bacteriological and mycological tests tested negative, and the patient's response to antibiotics was poor. Skin biopsy of the subcutaneous induration on the left forearm showed hemorrhage, neutrophil and lymphocyte infiltration of the deep dermis, and neutrophilic lobular panniculitis, without any signs of vasculitis (Fig. 1d, e). The lesions on the extremities and sacral area improved without up-titration of the dose of PSL.
(a) Well-demarcated deep ulcer on the central vein catheter insertion site. (b) Painful erythematous nodules on the forearm (arrow). (c) Ulcerative lesion on the sacral area. (d) Histopathology examination showing lobular panniculitis (H–E, ×20). (e) Higher magnification showing neutrophil infiltration inside the fat tissue (H–E, ×200).
In the current case, deep ulcers at the central venous catheter insertion site on the right neck were considered a pathergy reaction, a characteristic feature of PG. There were no ulcerative lesions suggestive of PG on any part of the body other than the neck. After 2 months, painful subcutaneous erythematous nodules appeared on the extremities, and a skin biopsy revealed the presence of neutrophilic lobular panniculitis. Because neither septal panniculitis nor Miescher radial granuloma was seen, erythema nodosum was excluded. PG and neutrophilic panniculitis are both categorized as deep neutrophilic dermatoses,1 suggesting a shared pathogenesis. Neutrophilic lobular panniculitis is observed in subcutaneous Sweet's syndrome. PG and Sweet's syndrome are the representative diseases of neutrophilic dermatosis, and both diseases often clinically present with similar features, which are difficult to differentiate, especially in patients with hematologic disorders.2–4 Such overlapped or atypical cases have been reported under the term ‘neutrophilic dermatosis of myeloproliferative disorders’, suggesting a linking of entities of both disorders in a continuous pathologic spectrum.5 Although the cervical ulcer was not biopsized in the present case, ulcerative neutrophilic panniculitis cannot be ruled out.
The VEXAS syndrome (vacuoles, E1 enzyme, X-linked, autoinflammatory, somatic) is an inflammatory disease due to somatic UBA1 variants presenting with myelodysplasia, and autoinflammatory symptoms including chondritis, vasculitis, and neutrophilic dermatosis.6 The VEXAS syndrome was listed as a differential disease because of the common complication of neutrophilic dermatosis and myelodysplastic syndrome. However, it was ruled out in this case because the granulocyte progenitor cells did not contain cytoplasmic vacuoles in the bone marrow biopsy. The current case of myelodysplastic syndrome presented with different clinical phenotypes such as deep ulcer, and painful erythematous subcutaneous nodules at different points in time, both of which were due to activated neutrophils.
Conflict of interestsThe authors declare that they have no conflict of interest.