An 82-year-old man with hypertension, a hiatal hernia, and osteoporosis was seen in outpatients for a painful, localized, nonbleeding, nonulcerated lesion on the left temple that had first appeared 4 months earlier.
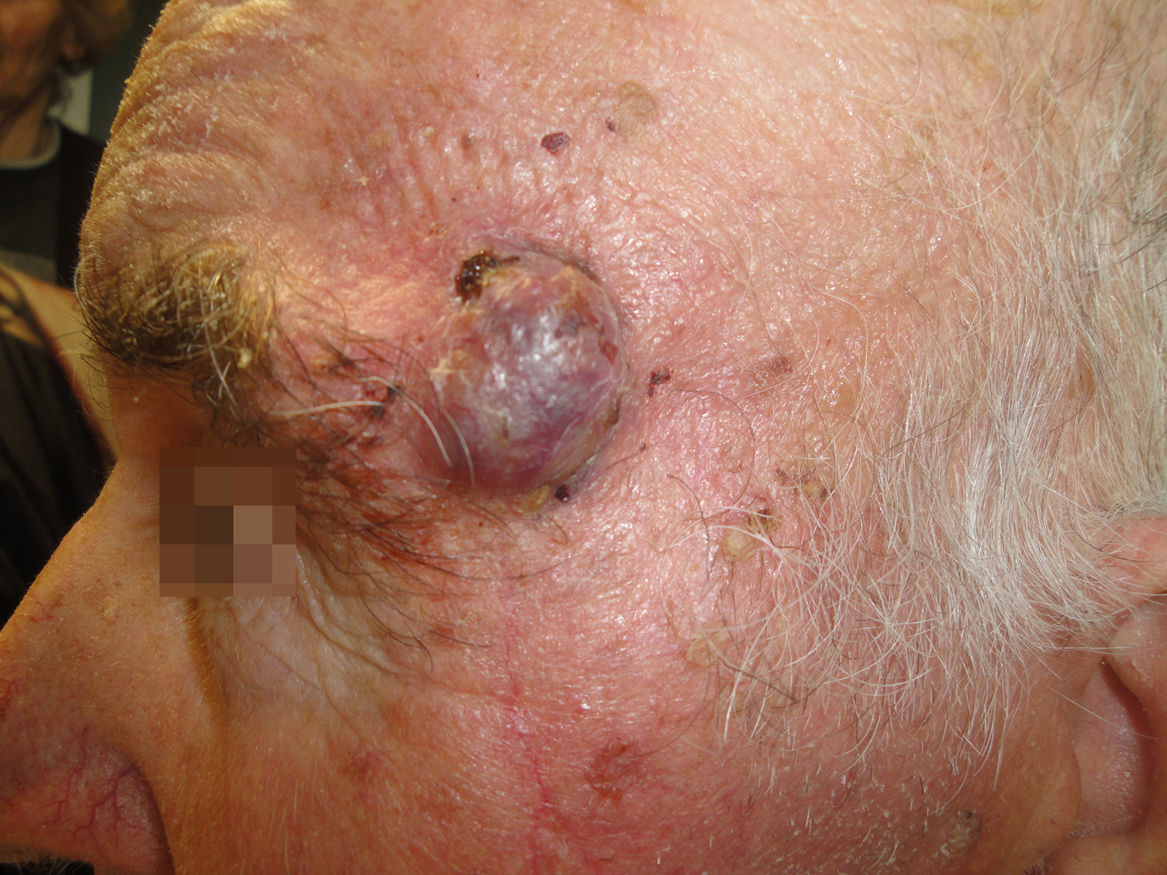
Physical ExaminationPhysical examination revealed a 2-cm erythematous-violaceous exophytic tumor on the left temple with well-defined borders. The lesion extended to the inferior lateral edge of the eyebrow (Fig. 1). Palpation revealed that the lesion was adherent to the deeper tissue layers. There were no palpable locoregional lymph nodes.
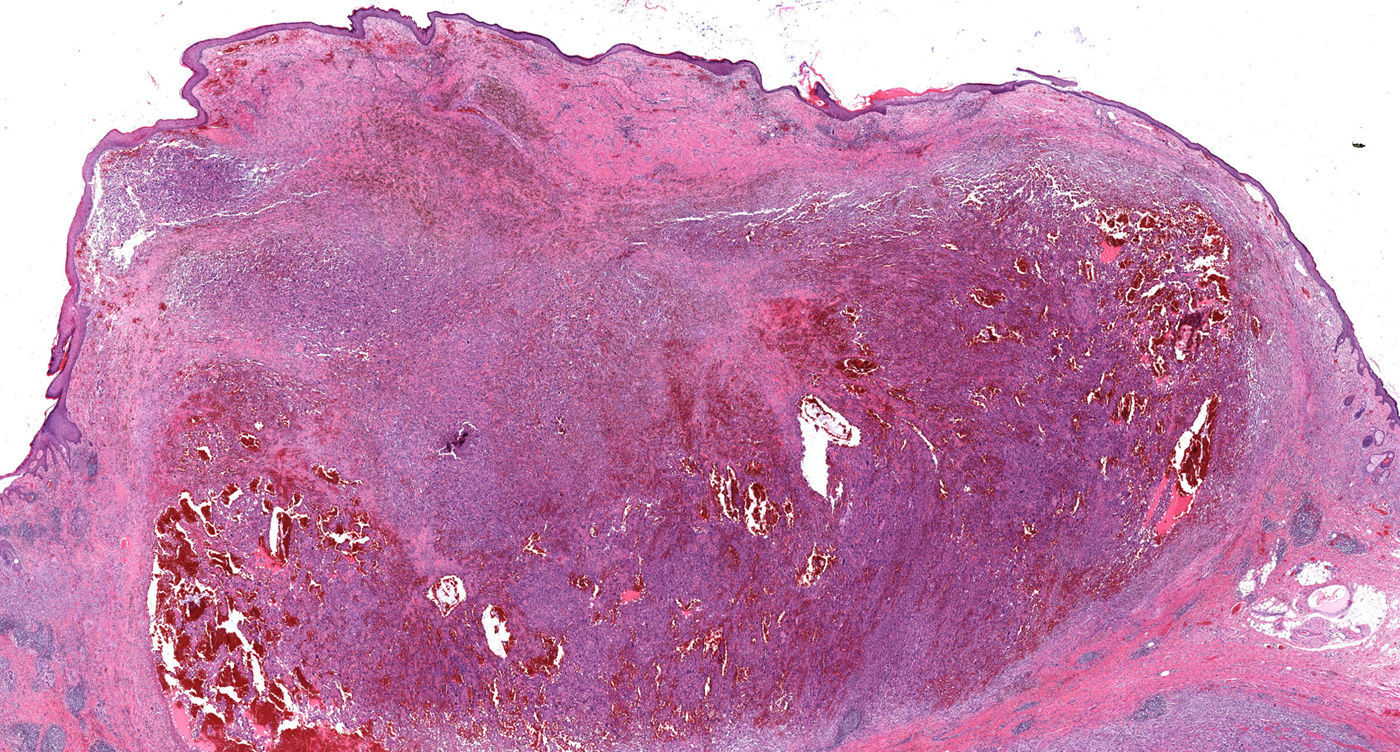
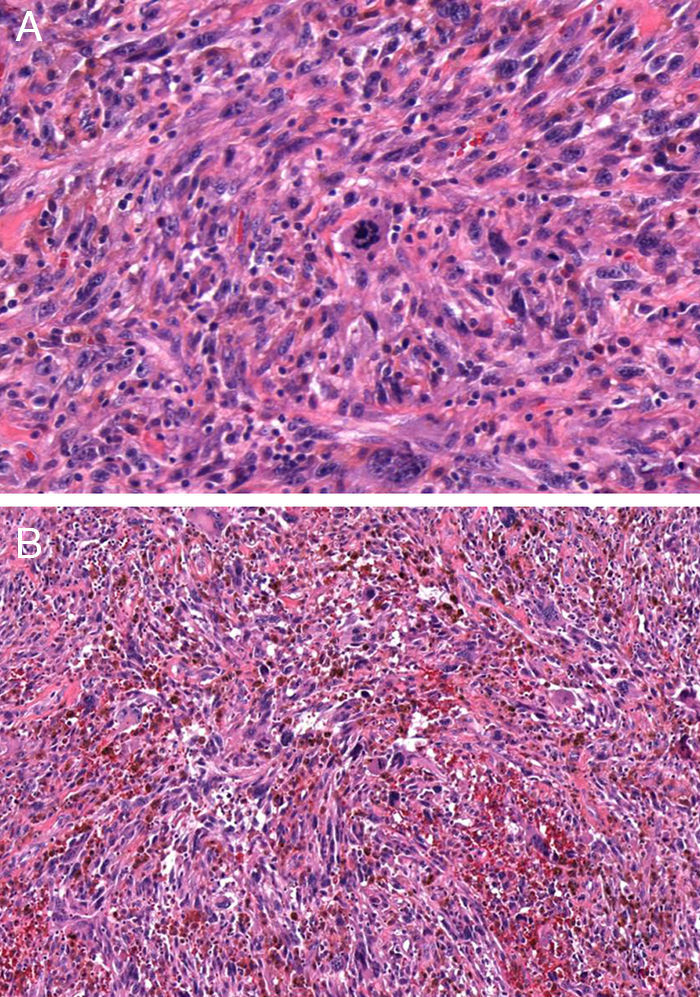
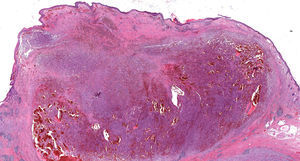
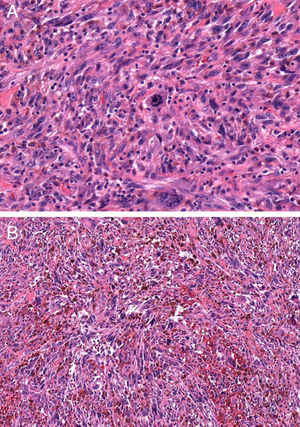
HistopathologyHematoxylin-eosin staining of a biopsy specimen revealed an orthokeratotic epidermis and a dermal infiltrate of elongated pleomorphic cells, intermixed with other cells with rounded and irregular nuclei as well as abundant aberrant mitotic figures (Fig. 2 and Fig. 3A). This infiltrate formed a storiform pattern over a collagenized fibrous stroma with striking vascular structures (Fig. 3B). Immunohistochemical staining was positive for CD68 and CD31 and showed focal positivity for S100, isolated positivity for vimentin, and a Ki-67 proliferation index of nearly 70%. Other stains, including for smooth muscle actin, desmin, cytokeratin AE1/AE3, CD34, CD10, common leukocyte antigen, HMB-45, and Melan-A, were negative.
What Is Your Diagnosis?
DiagnosisPleomorphic dermal sarcoma.
Clinical Course and TreatmentThe lesion was excised but the surgical margins were not clear. Therefore, slow Mohs surgery was performed and complete excision was achieved with a single stage of surgery. The defect was closed with a full-thickness skin graft.
A staging study revealed swelling of a left retroauricular lymph node, which was shown by biopsy to be diseased. The case was evaluated by the tumor committee and complementary treatments were ruled out. After 18 months of follow-up, there had been no local recurrence and no changes in the course of the disease.
CommentSarcomas are neoplasms of mesenchymal origin that are more common in adults. Classification and prognosis are determined by cell lineage.
Recent advances in immunohistochemistry and molecular genetics have brought about a gradual decrease in the incidence of the tumor previously known as malignant fibrous histiocytoma and an increase in the incidence of more specific entities.1,2 In the latest classification of bone and soft tissue tumors, published by the World Health Organization (WHO) in 2013, the term malignant fibrous histiocytoma was replaced by undifferentiated pleomorphic sarcoma.1,3 This is a diagnosis of exclusion for fibrohistiocytic neoplasms that cannot be clearly differentiated using the diagnostic techniques currently available. It is important to avoid confusion between the tumor now known as undifferentiated pleomorphic sarcoma and the similarly named pleomorphic dermal sarcoma.4–6
Pleomorphic dermal sarcoma typically appears in men in the seventh or eighth decade of life as a rapidly growing dermal nodule with necrotic and hemorrhagic areas, usually on sun-exposed sites such as the head and neck.4,5 Characteristically, this tumor presents pleomorphic epithelioid cells and atypical spindle cells with numerous mitotic figures and extensive areas of ulceration and necrosis, as well as involvement of deep tissues and vascular and perineural invasion, which distinguishes it from atypical fibroxanthoma.4–6 Immunohistochemistry is essential to rule out other entities such as melanocytic tumors, malignant nerve sheath tumors, poorly differentiated squamous cell carcinomas, angiosarcomas, leiomyosarcomas, and Merkel cell carcinoma.2,6
Metastatic spread occurs in an estimated 10% of cases and local recurrence in 30% of cases.4–6 Data from large case series are not available due to the multiple nomenclature changes.
The first-line treatment is conventional surgery with tumor-free margins or Mohs surgery.4,6 As in other fibrohistiocytic tumors, there are no consensus recommendations on the treatment of metastatic disease or follow-up.
This case underscores the need to be familiar with and apply the new WHO classification, which will make it possible to standardize the diagnosis of soft tissue tumors, thereby improving clinical management of these neoplasms. The case also highlights the importance of immunohistochemistry in the diagnosis of these tumors and the need to perform staging studies to assess the possibility of distant metastasis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The authors would like to thank Dr Rodríguez Peralto and Dr Enguita Valls of the Anatomical Pathology Service of the Hospital Universitario 12 de Octubre for their invaluable help.
Please cite this article as: Varas-Meis E, Otero-Rivas MM, Rodriguez-Prieto MÁ. Tumoración excrecente en sien izquierda. Actas Dermosifiliogr. 2017;108:771–772.