Cutaneous lesions specific to systemic sarcoidosis may vary in terms of their clinical appearance and can mimic many skin conditions.1 Ichthyosiform sarcoidosis is one of the least common sarcoidosis-specific cutaneous manifestations.1,2
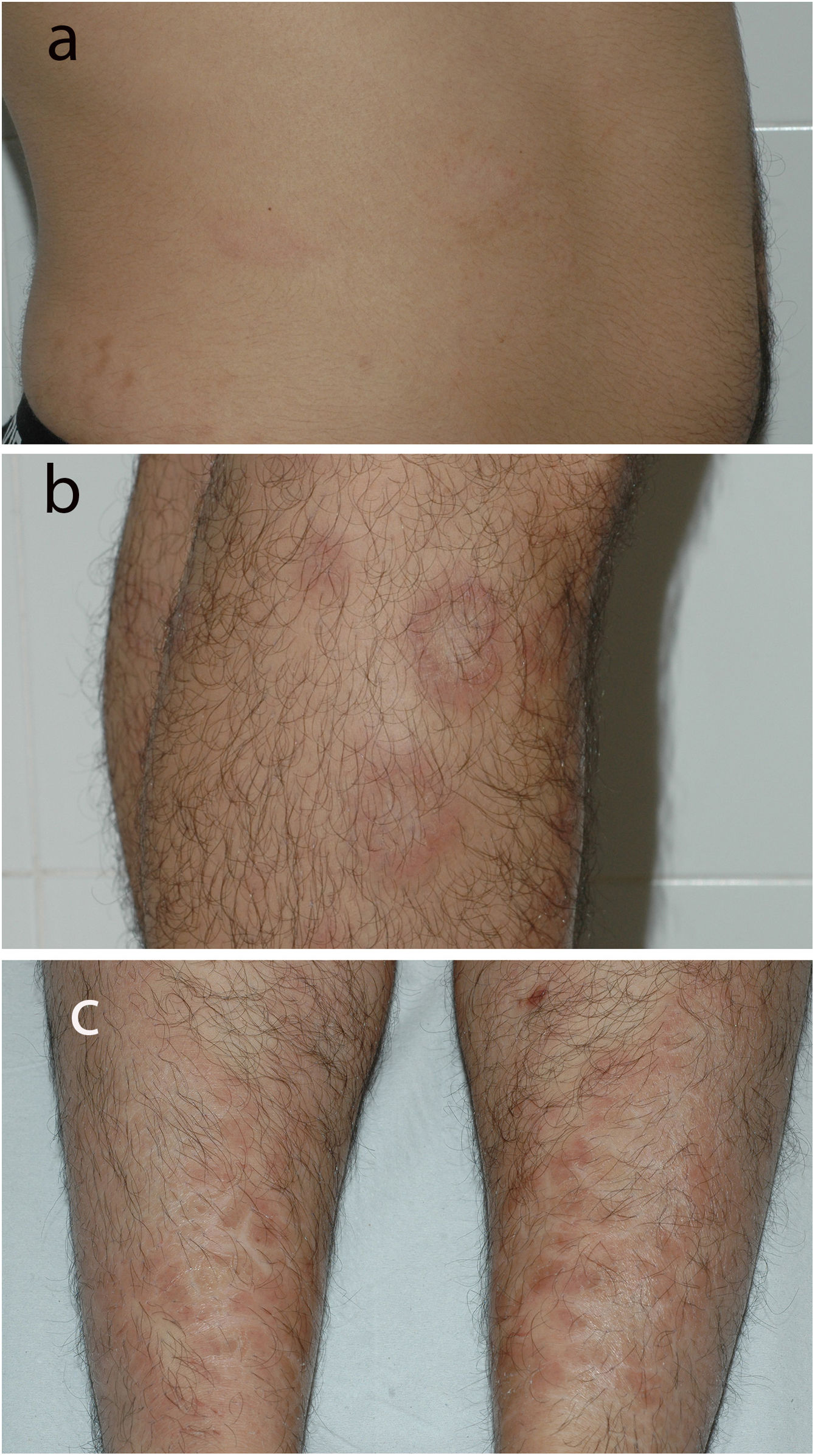
A 25-year-old man from Venezuela and resident in Spain for the last 15 years consulted for annular erythematous lesions located mainly on the lower limbs. The lesions were accompanied by thick scales with an ichthyosiform appearance in the pretibial area. The patient's clinical history was unremarkable. He reported that the skin lesions, which were asymptomatic, had first appeared on both lower limbs 4 months earlier. He had not experienced fever, cough, or other systemic symptoms. None of his relatives had had similar lesions. Examination revealed annular erythematous lesions in the proximal aspect of the lower limbs, with a few also visible on the right abdominal flank (Fig. 1A and B). On the pretibial area and ankles, the skin was affected by diffuse erythema covered by large polygonal ichthyosiform scales (Fig. 1C). Biopsy of one of the annular lesions on the knee revealed a lymphohistiocytic inflammatory infiltrate with poorly formed granulomatous structures arranged in a perivascular, perineural, and periadnexal pattern (Fig. 2A and B). Further biopsy of another lesion on the thigh revealed dermal sarcoid granulomas marked by clear syringotropism (Fig. 2C). Staining for acid-alcohol-fast bacilli yielded negative results. Biopsy of an ichthyosiform lesion on the ankle also revealed the presence of sarcoid granulomas in the dermis, as well as orthokeratotic hyperkeratosis in the epidermis (Fig. 2D). Physical examination revealed no alterations in sensitivity, and staining for acid-alcohol-fast bacilli in smears from the nasal cavity and earlobe were negative. Serology testing for syphilis was negative. Angiotensin-converting enzyme values were high (139U/L [reference range, 8–52U/L]), the chest X-ray revealed bilateral enlarged hilar lymph nodes, and the ophthalmological examination revealed choroidal granulomas.
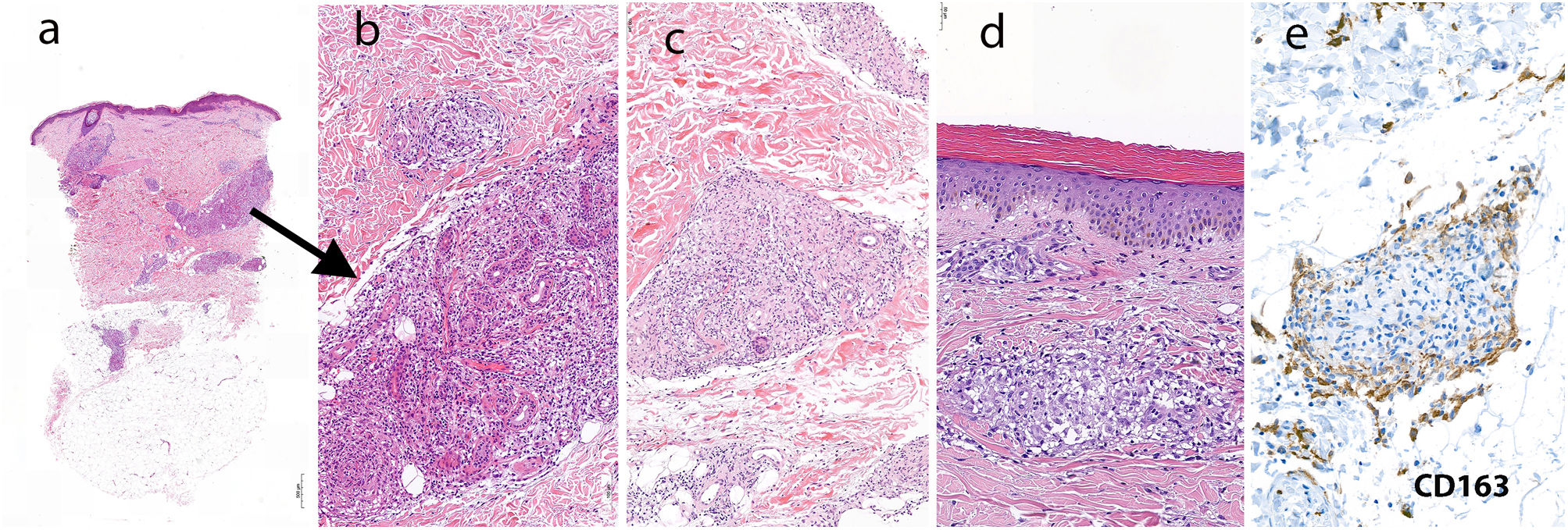
Histopathology of lesions on the right knee at low magnification with the presence of a lymphohistiocytic inflammatory infiltrate and poorly formed granulomatous structures (hematoxylin–eosin, ×20). A, Increased magnification better reveals the granulomatous infiltration of the eccrine glands (hematoxylin–eosin, ×100). B, Histopathology of the lesions on the thigh, with infiltration of the eccrine glands by sarcoid granulomas (hematoxylin–eosin, ×100). C, Histopathology of pretibial ichthyosiform lesions showing orthokeratotic hyperkeratosis and sarcoid granulomas in the dermis (hematoxylin–eosin, ×100) (D). E, Immunohistochemistry for CD163 showing a high density of CD163-positive cells in the interstitial area surrounding the epithelioid granulomas (CD163, ×100).
Macrophages in cutaneous lesions in sarcoidosis were recently reported to be positive for CD163 in patients with systemic involvement.3 Consistent with the study in our patient with systemic sarcoidosis, immunohistochemistry revealed a high density of CD163+ cells in the interstitial area surrounding the epithelioid granulomas.
Ichthyosiform sarcoidosis is clinically characterized by large gray or brown polygonal scales located mainly in the pretibial area.4 Only 34 cases of ichthyosiform sarcoidosis have been reported. Most affected Black patients, followed by Asian patients, with only 4 cases reported in White patients.2 Ichthyosiform lesions may be erroneously diagnosed as dry skin, and some authors believe that they may be more prevalent than previously thought, since patients with ichthyosiform sarcoidosis may present other, more apparent types of cutaneous lesions in sarcoidosis.4
Histologically, ichthyosiform sarcoidosis is characterized by hyperkeratosis, acanthosis, and a diminished granular layer, all of which occur alongside sarcoid granulomas in the underlying dermis.4 In some published case reports, the authors stress that the granulomas tend to accumulate around the eccrine glands.4,5 Syringotropism has been thought to inhibit sweating by blocking or obstructing the eccrine duct, thus leading to xerosis and epidermal abnormalities.3 In some patients, a diminished sweating response to thermal stimuli has been observed.5 Hansen disease can also lead to sweating abnormalities, annular lesions, and ichthysiform lesions similar to those we report here.6 The differential diagnosis with sarcoidosis may prove difficult, since both conditions may be characterized by dermal granulomas arranged in a perineural fashion.7 Furthermore, in leprosy, development of ichthyosiform lesions has been thought to result from defective functioning of the eccrine glands owing to reduced hydration of the stratum corneum.6
In the patient we describe, sarcoid granulomas infiltrated the eccrine glands. In addition, the perineurally arranged granulomas we identified may have interfered with the innervation of these glands. The findings for the present case support the hypothesis that ichthyosiform lesions in sarcoidosis could be associated with granulomatous infiltration of the eccrine glands or interference in their innervation.
Conflicts of InterestThe authors declare that they have no conflicts of interest.