The negative impact of psoriasis on patient quality of life can be as important as the physical consequences of the disease. We could assume that clearance of the disease would also lead to an improvement in its psychosocial impact. The present study assesses the psychological state of patients with psoriasis receiving systemic treatment in a psoriasis unit, especially those with mild or no disease involvement.
MethodsWe performed a cross-sectional, observational, noninterventional epidemiological study of 2 cohorts (cases and controls). The patients self-completed demographic data and 4 questionnaires (Rosenberg Self-Esteem Scale, Skindex-29, HADS, and COPE-28 questionnaire) at a single visit.
ResultsWe recruited 111 patients diagnosed with psoriasis and 109 control patients. In self-esteem, the mean and standard deviation (SD) score was 33.5 (4.8) for the psoriasis group and 33.3 (6.7) for the control group, with no significant differences. In the Skindex-29, the mean score for the psoriasis group was almost 3 times higher than that of the control group (30 vs 11). Significant differences were found in the HADS scores of both groups (12.7 vs 9.0, P<.001). The mean HADS-A scores were 8.0 (4.78) for the psoriasis group compared with 5.7 (3.8) for the control group (P<.001). In the case of HADS-D, the scores were 4.7 (3.9) compared with 3.2 (3.1) (P<.004), respectively.
ConclusionsOur findings indicate that it is necessary to assess the psychological state of patients with psoriasis, because psychological effects persist even in cases where the disease is almost totally controlled.
El impacto negativo que la psoriasis tiene en la calidad de vida del paciente puede ser tan importante como sus consecuencias físicas. Podríamos suponer que el blanqueamiento de la enfermedad conllevaría también una mejoría de su impacto psicosocial. El presente estudio valora el estado psicológico de los pacientes con psoriasis controlados con tratamiento sistémico en una Unidad de Psoriasis, especialmente en aquellos con una afectación leve o nula de la enfermedad.
MétodosEstudio epidemiológico observacional y trasversal, sin intervención, con dos cohortes (casos y controles). Los pacientes autocompletaron datos demográficos y 4 cuestionarios (Cuestionario de autoestima de Rosenberg, Skindex-29, HADS y COPE-28) en una única visita.
ResultadosSe reclutaron 111 pacientes diagnosticados de psoriasis y 109 pacientes control. En autoestima, el promedio y la desviación estándar (DE) del grupo de psoriasis fue de 33,5 (4,8) y de 33,3 (6,7) para el grupo control, sin diferencias significativas. En el Skindex-29, la puntuación media del grupo de pacientes con psoriasis fue casi 3 veces mayor que la media del grupo control (30 vs 11). Se encontraron diferencias significativas en las puntuaciones del HADS de ambos grupos (12,7 vs 9,0; p<0,001). Las puntuaciones promedio del HADS-A fueron de 8,0 (4,78) en el grupo de psoriasis frente a 5,7 (3,8) en el grupo control (p<0,001), mientras que las del HADS-D fueron de 4,7 (3,9) frente a 3,2 (3,1) (p<0,004), respectivamente.
ConclusionesLos resultados obtenidos indican que es necesario medir el estado psicológico de nuestros pacientes con psoriasis, pues incluso con un control casi total de la enfermedad la afectación psicológica permanece.
Psoriasis is a chronic disease that affects 2% of the population in Spain.1 It is characterized by marked clinical heterogeneity with periods of fluctuation in disease activity.
The negative impact of psoriasis on patient quality of life (QOL) is well documented in the literature, thus supporting the notion that the psychosocial impact of psoriasis is as important as its physical consequences and contributes to morbidity.2 The fact that psoriasis mainly affects the skin can have a negative impact on body image and decrease patients’ self-esteem, self-confidence, and well-being.3
Furthermore, given the chronic nature of psoriasis, the patient must face the various demands and challenges presented by the disease itself. Chronic diseases usually affect several areas of life, and their impact on QOL can lead to depression, anxiety, and stress-related disorders, and even suicidal behavior.3–5 The prevalence of anxiety in psoriasis ranges from 7% to 48%.6 The prevalence of depression in psoriasis ranges from 6% to 62%. Data from a meta-analysis show that the percentage of patients with depressive symptoms measured using specific questionnaires is around 28%.4
When we analyze the coping strategies of patients with psoriasis, we see that the most common are planning, active coping, acceptance, and positive reframing of the disease. The least frequent are alcohol abuse, religion, and denial of the disease.7 The patients with the best mental health and QOL are those who more often use the most normalizing and optimistic coping options.7
An improvement in the severity of the disease, measured according to the decrease in the Psoriasis Area and Severity Index (PASI), can be accompanied by an improvement in psychological well-being.8 Therefore, we might think that any clinical improvement achieved through treatment would be accompanied by an improvement in disease-related psychological factors. However, our daily experience indicates that this is not always the case. Therefore, we think that the psychological involvement observed before the disease is controlled with therapy continues to be present in some way despite the improvement in skin lesions.
The main objective of the present study was to evaluate the psychological status of patients taking systemic treatment monitored at our psoriasis unit. Our secondary objective was to evaluate the psychological impact of the disease on a subgroup of patients with mild or no disease involvement.
MethodsDesignWe performed an epidemiological, observational, cross-sectional, noninterventional study of 2 cohorts (cases and controls). The study was approved by the local ethics committee. The participants were recruited consecutively at the dermatology clinic, where they were informed of the main objective of the study and signed the informed consent document. All of the patients completed the questionnaires in the waiting room after the visit.
ParticipantsWe recruited 111 patients with psoriasis who fulfilled the following criteria: plaque psoriasis under systemic treatment, age ≥ 18 years, no or controlled psoriatic arthritis, and follow-up at our psoriasis unit. In addition, patients had to have attended consecutively between April 2015 and April 2016 and voluntarily agree to participate in the study. We excluded patients with other types of psoriasis, patients aged < 18 years, those who had difficulty completing the questionnaires, and those with another chronic dermatological disease, as well as those who also had arthritis that was not clinically controlled. The control group included patients aged ≥ 18 years who came to the clinic with a trivial condition (e.g., evaluation of nevi, seborrheic keratosis, and verrucae) during the same observation period and did not have a family or personal history of psoriasis.
InstrumentsBoth groups completed the Rosenberg Self-Esteem Scale, the COPE-28 questionnaire on strategies for coping, Skindex-29, and the Hospital Anxiety and Depression Scale (HADS). We obtained demographic data, and patients in the study cohort underwent the PASI assessment always with the same observer. The questionnaires were completed and the PASI measured on the same day as the visit.
The Rosenberg Self-Esteem Scale is one of the most widely used for measuring self-esteem. It includes 10 items focusing on feelings of respect for and acceptance of oneself. It is scored between 10 and 40.9
COPE-28 is the Spanish version of the Brief COPE by Carver10 (1997), as drafted by Morán et al.11 (2010). It is a multidimensional inventory with 28 items and 14 subscales that is used to evaluate different ways of responding to stress.
The Skindex-29 questionnaire was adapted in Spanish by Jones-Caballero et al.12 for determination of participants’ QOL with respect to their skin. The questionnaire is self-administered and comprises 3 dimensions: function (12 items), emotions (10 items), and symptoms (7 items). The score of each dimension is obtained by transforming the sum of the responses on a linear scale of 100 ranging from 0 (absence of an impact on health-related QOL [HRQOL]) to 100 (maximum impact on HRQOL). A global score is obtained using this transformation.
Lastly, HADS is a self-administered questionnaire comprising 14 items that was developed to detect the possible presence of anxiety and depression in the context of nonpsychiatric outpatients. It comprises 2 subscales (anxiety [HADS-A] and depression [HADS-D]), each comprising 7 items, where patients have to describe their feelings during the previous week, with a maximum score of 21 on each subscale. HADS has different cutoff points for determining the probability of an emotional disorder. In the present study, we used the original cutoff proposed by Zigmond and Snaith for each of the subscales independently: a score of 8-10 represented possible presence of the disorder and a score of ≥11 pointed to a clinical problem.13,14 The questionnaire is a rapid screening instrument—but not a diagnostic instrument—that is used to facilitate and speed up referral of the patient to mental health care for appropriate evaluation, diagnosis, and treatment if applicable.
Statistical analysisIn descriptive terms, the quantitative variables were processed by analyzing measures of central tendency and dispersion: mean (standard deviation) for normally distributed variables and median (interquartile range) for nonnormally distributed variables. The Shapiro-Wilk test was used verify the normality of the quantitative variables. The frequency and percentage of the qualitative variables were calculated. The t test was used to compare continuous variables; the Mann-Whitney test was used to compare ordinal variables. The Pearson correlation coefficient was calculated to verify the association between quantitative variables, and the Spearman correlation coefficient was used to compare the association between ordinal variables. The Fisher exact test was used to compare qualitative variables. Statistical significance was set at P < .05 (α=0.05). The statistical analysis was performed using R Core Team (2017 version 3.1.2).
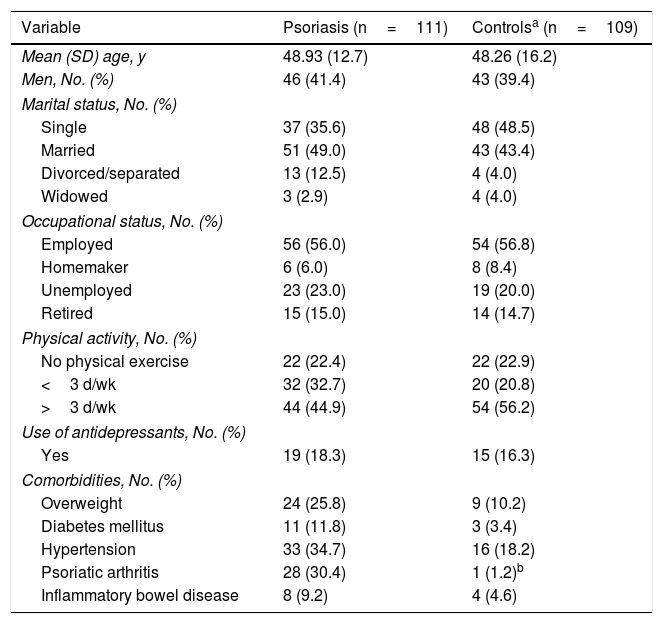
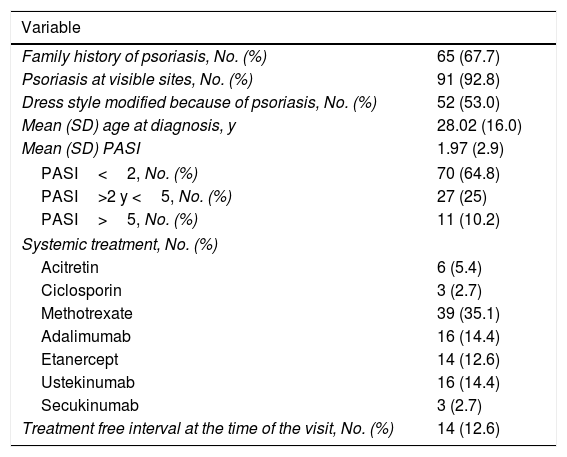
ResultsClinical dataA total of 220 patients agreed to participate in the study: 111 cases and 109 controls. Table 1 summarizes the demographic findings for both groups: comorbidities were similar, except for arthritis, which was more frequent in the cases. Table 2 summarizes the specific characteristics of the group of patients with psoriasis. The mean (SD) score in the PASI was 1.97 (2.91), indicating that disease was controlled for many patients in this group.
Sociodemographic Characteristics of Patients With Psoriasis (Cases) and Controls.
| Variable | Psoriasis (n=111) | Controlsa (n=109) |
|---|---|---|
| Mean (SD) age, y | 48.93 (12.7) | 48.26 (16.2) |
| Men, No. (%) | 46 (41.4) | 43 (39.4) |
| Marital status, No. (%) | ||
| Single | 37 (35.6) | 48 (48.5) |
| Married | 51 (49.0) | 43 (43.4) |
| Divorced/separated | 13 (12.5) | 4 (4.0) |
| Widowed | 3 (2.9) | 4 (4.0) |
| Occupational status, No. (%) | ||
| Employed | 56 (56.0) | 54 (56.8) |
| Homemaker | 6 (6.0) | 8 (8.4) |
| Unemployed | 23 (23.0) | 19 (20.0) |
| Retired | 15 (15.0) | 14 (14.7) |
| Physical activity, No. (%) | ||
| No physical exercise | 22 (22.4) | 22 (22.9) |
| <3 d/wk | 32 (32.7) | 20 (20.8) |
| >3 d/wk | 44 (44.9) | 54 (56.2) |
| Use of antidepressants, No. (%) | ||
| Yes | 19 (18.3) | 15 (16.3) |
| Comorbidities, No. (%) | ||
| Overweight | 24 (25.8) | 9 (10.2) |
| Diabetes mellitus | 11 (11.8) | 3 (3.4) |
| Hypertension | 33 (34.7) | 16 (18.2) |
| Psoriatic arthritis | 28 (30.4) | 1 (1.2)b |
| Inflammatory bowel disease | 8 (9.2) | 4 (4.6) |
Clinical Characteristics of Patients With Psoriasis.
| Variable | |
|---|---|
| Family history of psoriasis, No. (%) | 65 (67.7) |
| Psoriasis at visible sites, No. (%) | 91 (92.8) |
| Dress style modified because of psoriasis, No. (%) | 52 (53.0) |
| Mean (SD) age at diagnosis, y | 28.02 (16.0) |
| Mean (SD) PASI | 1.97 (2.9) |
| PASI<2, No. (%) | 70 (64.8) |
| PASI>2 y <5, No. (%) | 27 (25) |
| PASI>5, No. (%) | 11 (10.2) |
| Systemic treatment, No. (%) | |
| Acitretin | 6 (5.4) |
| Ciclosporin | 3 (2.7) |
| Methotrexate | 39 (35.1) |
| Adalimumab | 16 (14.4) |
| Etanercept | 14 (12.6) |
| Ustekinumab | 16 (14.4) |
| Secukinumab | 3 (2.7) |
| Treatment free interval at the time of the visit, No. (%) | 14 (12.6) |
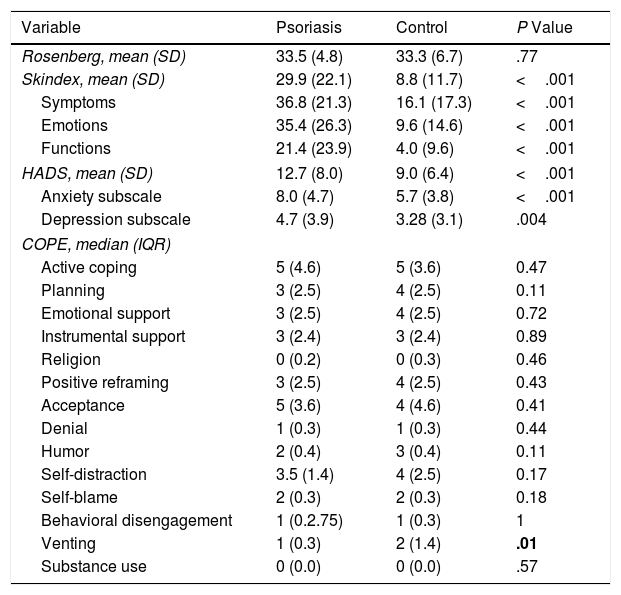
Table 3 provides the results obtained in each of the dimensions measured.
Results of the Scales.
| Variable | Psoriasis | Control | P Value |
|---|---|---|---|
| Rosenberg, mean (SD) | 33.5 (4.8) | 33.3 (6.7) | .77 |
| Skindex, mean (SD) | 29.9 (22.1) | 8.8 (11.7) | <.001 |
| Symptoms | 36.8 (21.3) | 16.1 (17.3) | <.001 |
| Emotions | 35.4 (26.3) | 9.6 (14.6) | <.001 |
| Functions | 21.4 (23.9) | 4.0 (9.6) | <.001 |
| HADS, mean (SD) | 12.7 (8.0) | 9.0 (6.4) | <.001 |
| Anxiety subscale | 8.0 (4.7) | 5.7 (3.8) | <.001 |
| Depression subscale | 4.7 (3.9) | 3.28 (3.1) | .004 |
| COPE, median (IQR) | |||
| Active coping | 5 (4.6) | 5 (3.6) | 0.47 |
| Planning | 3 (2.5) | 4 (2.5) | 0.11 |
| Emotional support | 3 (2.5) | 4 (2.5) | 0.72 |
| Instrumental support | 3 (2.4) | 3 (2.4) | 0.89 |
| Religion | 0 (0.2) | 0 (0.3) | 0.46 |
| Positive reframing | 3 (2.5) | 4 (2.5) | 0.43 |
| Acceptance | 5 (3.6) | 4 (4.6) | 0.41 |
| Denial | 1 (0.3) | 1 (0.3) | 0.44 |
| Humor | 2 (0.4) | 3 (0.4) | 0.11 |
| Self-distraction | 3.5 (1.4) | 4 (2.5) | 0.17 |
| Self-blame | 2 (0.3) | 2 (0.3) | 0.18 |
| Behavioral disengagement | 1 (0.2.75) | 1 (0.3) | 1 |
| Venting | 1 (0.3) | 2 (1.4) | .01 |
| Substance use | 0 (0.0) | 0 (0.0) | .57 |
Abbreviation: IQR, interquartile range.
The average score in self-esteem was 33.5 (4.8) for the psoriasis group and 33.3 (6.7) for the control group, with no significant differences. We observed that 18.5% of patients with PASI between 2 and 5 had low self-esteem (score below 25) compared with 5.5% in the control group (P=.056).
Quality of lifeThe mean score for psoriasis patients in Skindex-29 was almost 3 times greater than the mean score of the control group (30 vs 9), and all the comparisons in each of the dimensions were statistically significant (P<.001). The most affected dimensions in the study patients were symptoms (37 vs 16) and emotions (35 vs 9).
Coping strategiesThe coping strategies most commonly used by patients with psoriasis were active coping (5 vs 5) and acceptance (5 vs 4); statistical significance was only recorded for venting (P=.01). Appendix A (Supplementary Material) contains the definitions for each of the questionnaire scales and the COPE-28 questionnaire.
Anxiety and depressionStatistically significant differences in HADS were observed for the average scores in both groups (12.7 vs 9.0; P<.001). The HADS-A (anxiety) score was greater than the HADS-D (depression) score. The average scores on HADS-A were 8.0 (4.78) in the psoriasis group compared with 5.7 (3.8) in the control group (P<.001), whereas those in HADS-D the average scores were 4.7 (3.9) compared with 3.2 (3.1) (P<.004), respectively.
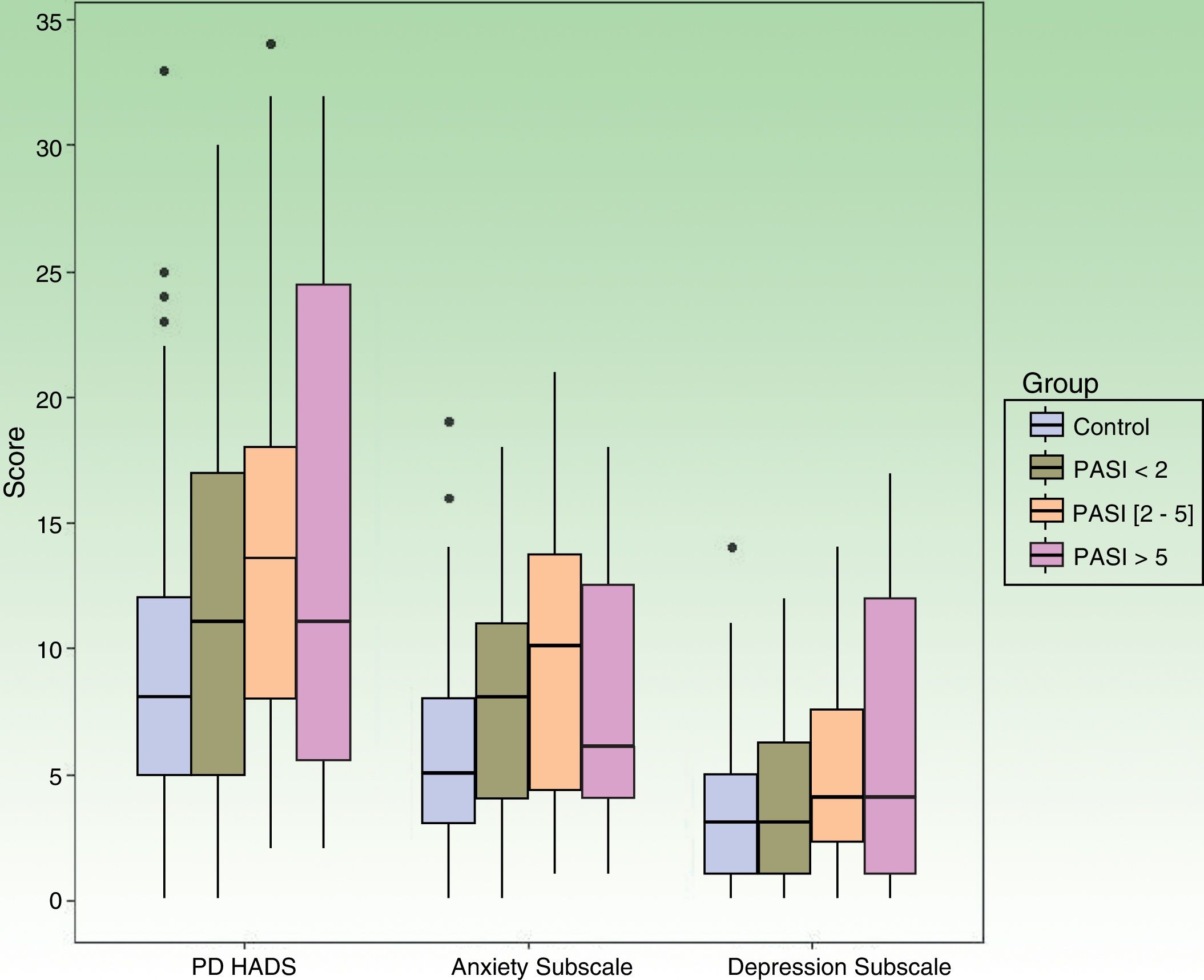
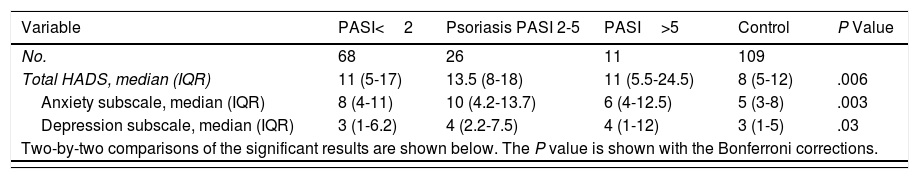
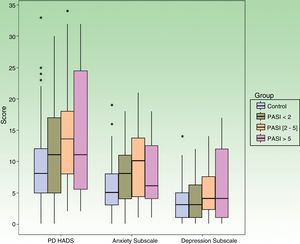
Table 4 shows data from the subanalysis according to the PASI score. We found significant differences in the probability of a HADS score compatible with clinical problems in all of the psoriasis groups (independently of the PASI score) and in all comparisons with respect to the controls (P=.006). In the case of HADS-A, there were significant differences in the probability of a score compatible with the clinical problem in all of the psoriasis groups compared with the controls (P=.003). In HADS-D, statistical significance was only detected in the comparison between the control group and patients with a PASI between 2 and 5 (Fig. 1).
HADS Score According to PASI Compared With Controls.
| Variable | PASI<2 | Psoriasis PASI 2-5 | PASI>5 | Control | P Value |
|---|---|---|---|---|---|
| No. | 68 | 26 | 11 | 109 | |
| Total HADS, median (IQR) | 11 (5-17) | 13.5 (8-18) | 11 (5.5-24.5) | 8 (5-12) | .006 |
| Anxiety subscale, median (IQR) | 8 (4-11) | 10 (4.2-13.7) | 6 (4-12.5) | 5 (3-8) | .003 |
| Depression subscale, median (IQR) | 3 (1-6.2) | 4 (2.2-7.5) | 4 (1-12) | 3 (1-5) | .03 |
| Two-by-two comparisons of the significant results are shown below. The P value is shown with the Bonferroni corrections. | |||||
| Variables/Comparisons | Control vs PASI<2 | Control vs PASI 2-5 | Control vs PASI>5 |
|---|---|---|---|
| Total HADS | 0.08 | 0.02 | 0.89 |
| Anxiety subscale | 0.06 | 0.01 | 0.83 |
| Depression subscale | 0.41 | 0.07 | 0.94 |
Abbreviations: HADS, Hospital Anxiety and Depression Scale; IQR, interquartile range.
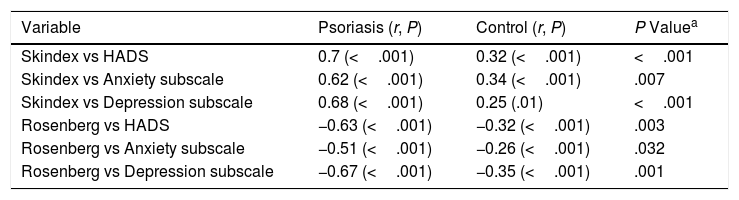
We also calculated the correlations between the results obtained in Skindex-29 and the Rosenberg Self-Esteem scale and compared them with HADS. We found a positive correlation between the values for Skindex-29 and HADS, both in the psoriasis group and in the control group. However, the correlation between the HADS and Rosenberg Self-Esteem scales was negative in both groups (Table 5).
Correlations Between Variables.
| Variable | Psoriasis (r, P) | Control (r, P) | P Valuea |
|---|---|---|---|
| Skindex vs HADS | 0.7 (<.001) | 0.32 (<.001) | <.001 |
| Skindex vs Anxiety subscale | 0.62 (<.001) | 0.34 (<.001) | .007 |
| Skindex vs Depression subscale | 0.68 (<.001) | 0.25 (.01) | <.001 |
| Rosenberg vs HADS | −0.63 (<.001) | −0.32 (<.001) | .003 |
| Rosenberg vs Anxiety subscale | −0.51 (<.001) | −0.26 (<.001) | .032 |
| Rosenberg vs Depression subscale | −0.67 (<.001) | −0.35 (<.001) | .001 |
Psychological involvement can be measured using various instruments. This variable has traditionally been evaluated using HADS. However, given that some areas are not covered by this questionnaire, we applied other instruments. In our study, we chose the most widely used instruments, namely, HADS, COPE-28, and the Rosenberg Self-Esteem Questionnaire, which enabled us to compare the results obtained.4,6,7
The chronic course of psoriasis is associated with many psychological conditions that we did not evaluate. Alexithymia and feelings of rejection, embarrassment, anger, and negativity3,15,16 are associated with severe psoriasis. However, this was not the case of the patients assessed in the present study, since their disease had almost fully cleared (PASI<2). Therefore, they were not the object of our study, which focused on the presence of symptoms of anxiety and depression. Although some studies have shown that improvement in the severity of psoriasis—measured as a reduction in PASI—is accompanied by an improvement in patients’ psychological status,8 the data obtained in our study seem to indicate the presence of psychological involvement irrespective of the degree of therapeutic control achieved that is considered acceptable in daily clinical practice (mean PASI, 1.97).
Self-esteem was not affected, except in patients whose psoriasis lesions persist (PASI 2-5; our study did not make it possible to evaluate this item in patients with PASI>5, since it was not a study objective). Kouris et al.17 recently revealed that the average score on the Rosenberg Self-Esteem Scale in patients with psoriasis was 14.75 (2.95). Given that psoriasis is a visible and evident disease, our finding is noteworthy, in that self-esteem is associated with body image, concept of self, and how one evaluates oneself. Therefore, it would be interesting to explore whether the impact of the disease is attenuated by the quality of the care received from health care personnel and/or the expectations offered to the patient with respect to complete clearance.
As for coping strategies, our findings are consistent with those reported in the literature: active coping is the most frequently used strategy, with some differences compared with the control group.7,18 Nevertheless, we cannot rule out the possibility that this result is associated with the potential bias resulting from the greater motivation of the study patients, as seen in their adherence to the care provided in our psoriasis unit. The venting subscale in COPE-28 refers to increased awareness of one's own emotional malaise, accompanied by a tendency to express or release these feelings. The finding of differences between the control group (which uses the subscale more frequently than the cases) could lead us to think that patients with psoriasis block this aspect. We were unable to find comparative data elsewhere with respect to this coping strategy; therefore, it would be interesting to explore this subject in greater detail in further studies.
The HRQOL scores recorded by our group were very similar to those found during the validation of the Spanish version of Skindex-29.12 Both studies show that the most affected scales are symptoms and emotions, although in our sample, the average scores are slightly lower (symptom scale, 37 in our study vs 42 in the study by Jones-Caballero et al12; emotions scale, 35 vs 38, respectively). This difference could be due to the fact that the study was not specifically designed to measure HRQOL in patients with psoriasis but was aimed at patients with skin diseases in general, including various inflammatory skin diseases.
The average scores on the HADS questionnaire (12.7 in the psoriasis group; P<.001) point to the presence of a clinical problem. If we use the cut-off point of Zigmond and Snaith,14 then 57% of patients with psoriasis have a HADS score above 11 (OR=2.467; P=.002), thus indicating some type of psychological involvement. Of these, 31.7% have scores consistent with anxiety, and 11.2% have scores consistent with depression. The mean score in the control group was also high (HADS>11, 34.9%); however, it is worth remembering that our control group did not comprise healthy individuals (as the patients have a dermatological disease, their levels of anxiety and depression could be affected, even if the disease is trivial) and was assessed in a health care setting. Other studies also report the presence of psychological disorders, with a prevalence of anxiety of 17.2% in patients with dermatological complaints compared with 11.1% in healthy controls, and a prevalence of depression of 10.1% compared with 4.3%, respectively.19 Our data show marked anxiety in patients with psoriasis, despite the fact that they have few or no symptoms, and illustrate the need for a holistic approach that goes beyond drug therapy.
The main limitation of our study is that the control group did not comprise healthy individuals but patients with disease (even trivial). Furthermore, the ongoing nature of follow-up prevented patients from completely disconnecting from the disease, since they were constantly reminded of their condition and had to face it at each visit. In addition, the low percentage of patients with total clearance (n=17; 15.7%) could represent a bias, thus leading us to consider whether it is the visual presence of the disease itself, and not its extension, that serves as a stigmatizing reminder for the patient. Our study is noteworthy because it includes a very broad sample of patients in clinical remission and is one of the few studies that analyze psychological impact in patients with psoriasis.
It seems appropriate that integrated health care of patients with psoriasis should include the use of objective tests to assess the presence of mood disorders. HADS could prove useful for verifying the status of patients and working on areas associated with emotional support.6 If the tests cannot be incorporated into our daily practice, then we should at least ask 2 simple questions about state of mind and anhedonia (“During the last 2 weeks, have you felt down, depressed, or without hope?” and “During the last 2 weeks, have you had little interest or pleasure in doing things?”).20,21
In conclusion, our results reflect the presence of psychological involvement in patients with psoriasis controlled with therapy, despite a substantial improvement in their skin lesions. Furthermore, a high percentage of the study patients with mild or no psoriasis still have symptoms of anxiety. Psychological attention is necessary as a complement to evaluate patients’ health status.22 We are considering performing a similar study in patients with PASI 0 to determine whether minimum skin involvement after treatment is sufficient to demonstrate psychological impact in patients with psoriasis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Álvarez MBM, Hernández GC, Quesada AG, Martín JMG. Medición del impacto psicológico en pacientes con psoriasis en tratamiento sistémico. Actas Dermosifiliogr. 2018;109:733–740.