Commercial topical medications for oral conditions are scarce and the vehicles used are not very suitable. Therefore, formulations containing active ingredients in vehicles specially designed for oral application must often be prepared. Drug compounding offers other advantages, including the possibility of combining several active ingredients in a single vehicle and prescribing drugs that are in short supply. In this article, we describe the main pharmaceutical formulations used to treat the most common diseases of the oral mucosa.
Los medicamentos industriales comercializados para uso tópico oral son muy escasos y con vehículos poco adecuados. En consecuencia, frecuentemente hay que recurrir a preparados magistrales que permitan aplicar principios activos en vehículos diseñados especialmente para su aplicación en la mucosa oral. La formulación magistral también permite incluir varios principios activos en un mismo vehículo y prescribir fármacos actualmente en desabastecimiento, entre otras ventajas. Describimos las principales fórmulas magistrales para el tratamiento de la patología de la mucosa oral más frecuente.
The anatomic and functional structure of the oral mucosa differs considerably from that of the skin. The specific permeability, moisture, and motility in this area make application of topical treatments difficult. Suitable vehicles are necessary for application in this area, although current commercially available therapeutic options are very limited. In daily clinical practice, lesions of the oral mucosa require treatment with compounded preparations in most cases.
Suitable Vehicles for the Oral MucosaThe almost complete lack of commercially available medications for use on the oral mucosa means that we sometimes have to turn to medications that are applied to the skin. When an emulsion is applied to the oral mucosa, it disappears quickly owing to the hydrophilic nature of this tissue and the fact that the area is constantly moving, thus hampering systemic absorption of the active ingredients. Very fatty vehicles, in contrast, are washed off and are difficult to apply at the appropriate location.1,2
Suitable vehicles for this area include the following:
- •
Oral adhesive excipient. Oral adhesive excipient consists of a lipid-based vehicle (petrolatum) containing a large number of hydrophilic gelling agents (e.g., sodium carboxymethyl cellulose, gelatin, pectin) that enable the vehicle to bind to the mucosa while facilitating slower release of the active ingredients to the area. However, they have a granular texture that patients sometimes find unpleasant. Contact lasts approximately 30 minutes, although the therapeutic effect may last longer. This approach makes it possible to treat localized lesions. The mucosa should be dried before application, and the patient should not eat or drink for at least 30 minutes after application.
- •
Oral adhesive gel. In this case, the vehicle is composed of polyols (mainly glycerin and sorbitol) combined with a gelling agent. Its affinity for the moist mucosal surface is lower than with oral adhesive excipient, as is its ability to adhere to the mucosa, although its texture and taste are better. Oral adhesive gel also enables treatment of localized lesions and is indicated for patients who do not tolerate the texture of oral adhesive excipient.
- •
Solutions and suspensions. This approach involves aqueous solutions containing active ingredients in a solution or suspension depending on the solubility of the active ingredients in an aqueous medium. They can be used to treat multiple lesions on the oral mucosa. In some cases, the solutions must be hydroalcoholic in order to enable incorporation of active ingredients such as nystatin and clotrimazole, although the ethanol content should be low so as not to irritate the mucosa.
- •
Buccal tablets. The dissolving capacity of these tablets is superior to that of conventional approaches, thus enabling slower release of the active ingredients.
- •
Lollipops. Lollipops have a polyethylene glycol base with a pleasant taste and a support that enables it to be applied like a sweet. This approach is particularly indicated in children.
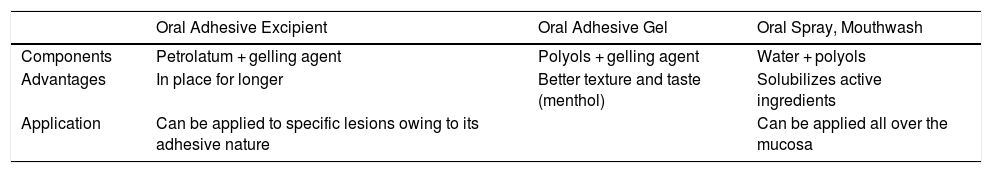
Table 1 shows the characteristics of the main vehicles.
Vehicles for the Oral Mucosa.
| Oral Adhesive Excipient | Oral Adhesive Gel | Oral Spray, Mouthwash | |
|---|---|---|---|
| Components | Petrolatum + gelling agent | Polyols + gelling agent | Water + polyols |
| Advantages | In place for longer | Better texture and taste (menthol) | Solubilizes active ingredients |
| Application | Can be applied to specific lesions owing to its adhesive nature | Can be applied all over the mucosa |
Oral lichen planus, especially the erosive form and symptomatic extensive reticular/hypertrophic forms. Corticosteroids are the treatment of choice, mainly clobetasol propionate 0.05%, although the 0.025% formulation has also proven to be effective.3 In fact, no differences were found in the response to treatment between systemic prednisone and topical clobetasol propionate in an adhesive medium.4 The most suitable vehicle is oral adhesive excipient, although if the patient cannot tolerate the texture, oral adhesive gel is a valid option. Multiple lesions should be treated with mouthwash based on a solution including dexamethasone. Since dexamethasone is water-soluble, unlike most corticosteroids, which are fat-soluble, it is the most appropriate option for incorporation in a solution. Concomitant antifungal treatment is safe and effective as prophylaxis for mucosal candidiasis.5
Several studies report the effectiveness of topical triamcinolone acetonide 0.1% applied 2 to 4 times daily,6 although in the clinical experience of the authors, it is much less effective than clobetasol propionate 0.05% applied twice daily.
When corticosteroids are applied in a solution, the patient should be advised to rinse with the solution in the mouth for a few minutes and not to swallow. It has been reported that patients prefer aerosol to mouthwash,7 although in our experience, mouthwash is more effective. Oral adhesive excipient should be the vehicle of choice where possible.
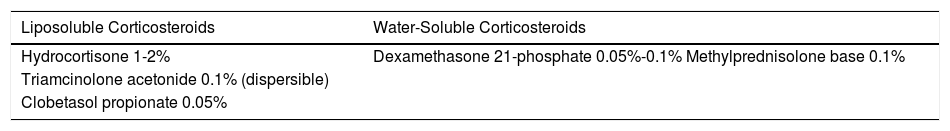
Table 2 shows the solubility of the main topical corticosteroids available for formulation as an oral solution. Interestingly, while unable to be formulated in an aqueous solution, triamcinolone acetonide can be included in a suspension.
Several studies have shown topical tacrolimus to be safe and effective, with very low systemic absorption and few local adverse effects.8 This agent is considered the next-best alternative to topical corticosteroids. The improvement begins to be noticed a few weeks after application, symptoms are controlled, the lesions resolve, and the drug is generally well tolerated, although the patient may experience a burning sensation, especially with the initial applications. Some authors believe that tacrolimus should be considered a first-line treatment for oral lichen planus,9 and various publications report on the use of commercial ointment or oral solutions. Compounding makes it possible to use a suitable vehicle, since commercially available ointment is unpleasant for patients and does not adhere well to the mucosa. We consider oral adhesive excipient to be the most appropriate vehicle.
Retinoids—retinoic acid 0.1% and 13 cis-retinoic acid 0.1%—are useful for restoring abnormal epithelial differentiation in keratotic forms, although they may lead to local irritation.10 We have found that combining the retinoid with the topical corticosteroid is well tolerated. Retinoic acid and 13 cis-retinoic acid seem to be equally effective. Furthermore, retinoids have been shown to be efficacious for the treatment of oral lichen planus compared both with placebo and with betamethasone.11,12
Topical ciclosporin in the form of an oily solution or in an adhesive medium is prescribed less and less frequently because of its high cost, possible systemic absorption, and potentially carcinogenic action.13 Most studies have not shown it to be more effective than topical corticosteroids.14 In patients with oral lichen planus that is refractory to standard therapy, we prefer topical rapamycin, even though we found only 1 published series of 7 cases of corticosteroid-resistant oral lichen planus treated with this active ingredient (complete remission of the flare-up was recorded in 4 patients).15 At present, the more widespread use of topical rapamycin in other diseases, such as angiofibroma, has reduced its cost and enabled it to be prescribed thanks to a compounded preparation with oral adhesive excipient as the most suitable vehicle.
Aloe vera can also be included in compounded preparations owing to its anti-inflammatory effect. It is also very well tolerated. While it has been suggested that application of Aloe vera in gel is significantly more effective than triamcinolone acetonide 0.1% in oral lichen planus,16 more studies are necessary to confirm this.17 In our experience, Aloe vera leads to partial response—and on rare occasions complete response—and can be considered a corticosteroid-sparing agent. Drug compounding enables it to be combined with other active ingredients.
A randomized placebo-controlled double-blind study of gel with chamomile 2% extract 3 times daily in patients with oral lichen planus showed that the chamomile extract improved symptoms and lesions.18 Chamomile extract is thought to have anti-inflammatory, antispasmodic, antibacterial, and antifungal effects. The active ingredients of chamomile include the essences azulene and chamazulene, as well as flavonoids, which are responsible for the properties of the extract. We do not recommend this agent in monotherapy, although we do recommend it as a vehicle for a topical corticosteroid or as coadjuvant treatment for symptoms.
Given its anti-inflammatory properties, tetracycline has proven successful for treatment of oral lichen planus in isolated cases,19 and it may act as an alternative when classic treatments have proven ineffective.
Photodynamic therapy can be considered an alternative in oral lichen planus that is resistant to standard therapy, although further well-designed studies are necessary to demonstrate its efficacy.20 It has been reported with both methylene blue 5% and with 5-aminolevulinic acid 5%-20%, both of which can be compounded.21–23 We lack experience with this approach, although it would only be viable using compounding.
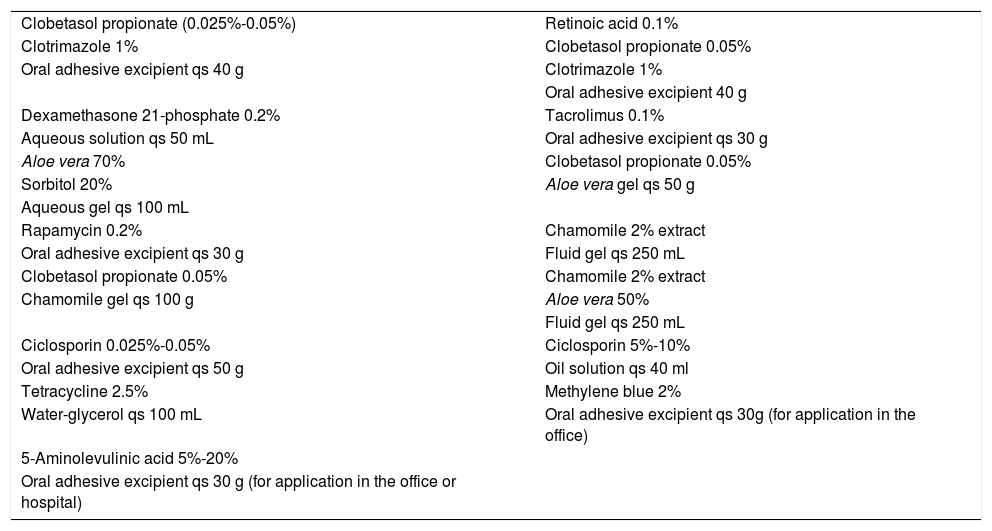
The formulas proposed for treatment of oral lichen planus are shown in Table 3.
Drug Compounding for Treatment of Oral Lichen Planus.
| Clobetasol propionate (0.025%-0.05%) | Retinoic acid 0.1% |
| Clotrimazole 1% | Clobetasol propionate 0.05% |
| Oral adhesive excipient qs 40 g | Clotrimazole 1% |
| Oral adhesive excipient 40 g | |
| Dexamethasone 21-phosphate 0.2% | Tacrolimus 0.1% |
| Aqueous solution qs 50 mL | Oral adhesive excipient qs 30 g |
| Aloe vera 70% | Clobetasol propionate 0.05% |
| Sorbitol 20% | Aloe vera gel qs 50 g |
| Aqueous gel qs 100 mL | |
| Rapamycin 0.2% | Chamomile 2% extract |
| Oral adhesive excipient qs 30 g | Fluid gel qs 250 mL |
| Clobetasol propionate 0.05% | Chamomile 2% extract |
| Chamomile gel qs 100 g | Aloe vera 50% |
| Fluid gel qs 250 mL | |
| Ciclosporin 0.025%-0.05% | Ciclosporin 5%-10% |
| Oral adhesive excipient qs 50 g | Oil solution qs 40 ml |
| Tetracycline 2.5% | Methylene blue 2% |
| Water-glycerol qs 100 mL | Oral adhesive excipient qs 30g (for application in the office) |
| 5-Aminolevulinic acid 5%-20% | |
| Oral adhesive excipient qs 30 g (for application in the office or hospital) |
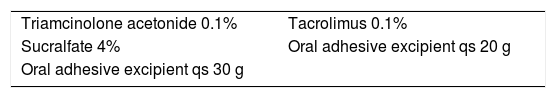
Geographic tongue does not usually require treatment, except when it is symptomatic. Symptomatic treatment is based on the application of topical corticosteroids, whether combined or not with lidocaine or sucralfate.24 Favorable experience has been reported with topical tacrolimus.25 These formulations are shown in Table 4.
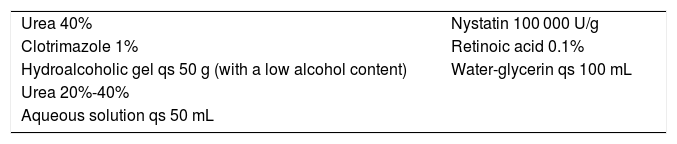
Black hairy tongueTreatment of black hairy tongue includes, first, suspension of drugs that are potentially involved, increased dental hygiene, and discontinuation of habits that predispose to this condition. Although only anecdotal cases with topical urea or retinoids have been published,26 our personal experience leads us to recommend brushing the affected area with a brush impregnated in a keratolytic agent (retinoic acid 0.1% or urea 40%) combined with an antifungal (clotrimazole or nystatin) owing to the possible implication of Candida albicans.27 Solutions with urea at a concentration higher than 30% are poorly stable and may release ammonia; therefore, the solution must be stabilized with mild acidification. The compounding pharmacist is aware of this problem. It is important to remember that if we wish to add an antifungal agent to an aqueous urea solution, the lack of solubility of the antifungal in water forces us to change the vehicle. One possible option is to formulate a gel with a low alcohol content (20%), to which clotrimazole can be added. A glycerin solution is recommended for nystatin. These formulas are shown in Table 5.
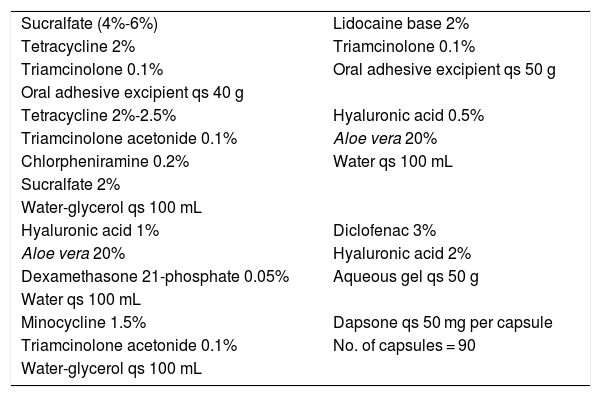
Aphthous stomatitisThe objective when choosing treatment for aphthous stomatitis is to accelerate healing and reduce pain. After evaluating the frequency of recurrences and severity, we should start the most appropriate therapy. Medical treatment is prescribed once possible triggers have been eliminated and/or associated abnormalities treated.
Topical corticosteroids are the first-line option. These shorten the duration of the ulcers and reduce pain. The drug and the corresponding vehicle are selected based on the severity and extension of the lesions; the most frequent are triamcinolone acetonide 0.1% and, to a lesser extent, dexamethasone 0.2%.28,29 Once again, it is important to bear in mind the solubility of the corticosteroids before selecting a vehicle (see above). The pharmaceutical industry currently markets hydrocortisone for topical oral use, although it is insufficient in cases of extensive or severe flare-ups, and it is precisely in these cases where we must turn to drug compounding.
One of the main advantages of drug compounding is the ability to include several active ingredients in a single vehicle. The ingredients that can be added to a corticosteroid are as follows:
- a)
Tetracyclines and their derivatives (minocycline, doxycycline): these agents contribute to healing thanks to their anti-inflammatory effect and ability to suppress collagenase activity.30,31
- b)
Sucralfate: this agent protects the gastric mucosa by forming a film over the ulcer, thus favoring healing.
- c)
Diphenhydramine: an antihistamine that exerts an anesthetic effect when applied on the oral mucosa.
- d)
Lidocaine: used to relieve pain.32
- e)
Diclofenac, which exerts an anti-inflammatory effect. The drug can be compounded in hyaluronic acid gel (the combination is superior to that of lidocaine and to hyaluronic acid in monotherapy33).
- f)
Aloe vera: shortens the time to healing of the ulcers and has been reported to relieve pain in anecdotal cases.34
- g)
Hyaluronic acid: acts as a demulcent, immunomodulator, and cell repair agent and protects the oral mucosa. It has proven to be safe and effective, both in recurrent aphthous stomatitis and in Behçet disease.35
The formulations proposed are shown in Table 6.
Drug Compounding in the Treatment of Aphthous Stomatitis.
| Sucralfate (4%-6%) | Lidocaine base 2% |
| Tetracycline 2% | Triamcinolone 0.1% |
| Triamcinolone 0.1% | Oral adhesive excipient qs 50 g |
| Oral adhesive excipient qs 40 g | |
| Tetracycline 2%-2.5% | Hyaluronic acid 0.5% |
| Triamcinolone acetonide 0.1% | Aloe vera 20% |
| Chlorpheniramine 0.2% | Water qs 100 mL |
| Sucralfate 2% | |
| Water-glycerol qs 100 mL | |
| Hyaluronic acid 1% | Diclofenac 3% |
| Aloe vera 20% | Hyaluronic acid 2% |
| Dexamethasone 21-phosphate 0.05% | Aqueous gel qs 50 g |
| Water qs 100 mL | |
| Minocycline 1.5% | Dapsone qs 50 mg per capsule |
| Triamcinolone acetonide 0.1% | No. of capsules = 90 |
| Water-glycerol qs 100 mL |
As for oral treatments, especially when prescribed to prevent recurrences, the first option is colchicine. However, if this is not effective, treatment with dapsone can be added.36 The formulation makes it possible to prescribe dapsone, which is not marketed in Spain outside the hospital setting, where it can be dispensed as a foreign medication.
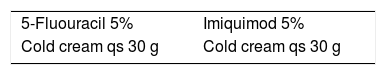
Actinic cheilitisPersonalized medication is necessary for patients with actinic cheilitis when alternatives such as physical therapy and surgery are not the first-choice options. The topical approach with the highest degree of evidence is 5-fluorouracil 5% in monotherapy,37 although photodynamic therapy combined sequentially with topical imiquimod 5% is the most appropriate approach after laser treatment and surgery.38 Since 5-fluorouracil 5% is not currently marketed and there is no suitable vehicle for it to be applied on the lips, drug compounding can be a therapeutic alternative. The preferred vehicle is cold cream, since this is an oil-in-water emulsion with a high lipid content. Imiquimod 5% or diclofenac 3%, may be alternatives, even though the level of evidence for these agents is low. When imiquimod was in short supply, the drug could continue to be used thanks to the compounded preparation. Table 7 provides detailed information for these preparations.
XerostomiaIndependently of treatment of the underlying cause of xerostomia and prevention of complications, the therapeutic strategy aims to produce saliva when there is still residual function of the salivary glands. Lemon juice is a natural stimulant, although it causes demineralization of the teeth. It is possible to prepare a 3.5% citric acid solution saturated with dicalcium phosphate in order to prevent demineralization.39
Pilocarpine has proven to be useful for treatment of hyposalivation, although its contraindications and adverse effects must be taken into account. In a recent study, oral pilocarpine at 15 mg/d in drops was compared with artificial saliva 3 times a day in a group of patients with Sjögren syndrome.40 Salivary flow improved significantly in the group treated with pilocarpine.40
Compounding pilocarpine enables lower doses to be prepared, if necessary, to prevent adverse effects and to provide a solution for patients who find it difficult to ingest capsules or tablets. Furthermore, this drug is very often in short supply.
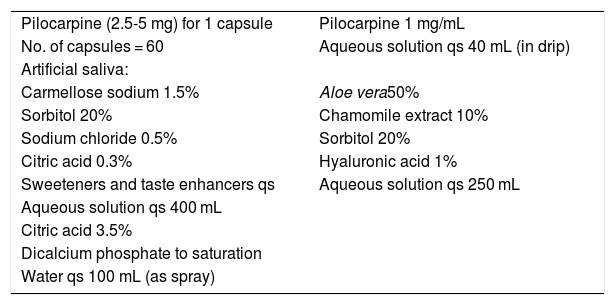
Patients who produce no or almost no saliva require artificial saliva. Given that there are many commercially available options, artificial saliva rarely has to be prepared as a compounded formulation. Preparations for artificial saliva can be tailored to the individual patient. Table 8 provides examples of preparations whose organoleptic properties best adapt to the patient’s taste.
Drug Compounding in the Treatment of Xerostomia.
| Pilocarpine (2.5-5 mg) for 1 capsule | Pilocarpine 1 mg/mL |
| No. of capsules = 60 | Aqueous solution qs 40 mL (in drip) |
| Artificial saliva: | |
| Carmellose sodium 1.5% | Aloe vera50% |
| Sorbitol 20% | Chamomile extract 10% |
| Sodium chloride 0.5% | Sorbitol 20% |
| Citric acid 0.3% | Hyaluronic acid 1% |
| Sweeteners and taste enhancers qs | Aqueous solution qs 250 mL |
| Aqueous solution qs 400 mL | |
| Citric acid 3.5% | |
| Dicalcium phosphate to saturation | |
| Water qs 100 mL (as spray) |
In addition to the classic saliva formulations with gelling agents and mineral salts, hydrating mouthwash with aloe vera and other extracts, polyols, and hyaluronic acid are well accepted by patients.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Iglesias-Sancho M, Llambí Mateos F, Salleras-Redonnet M. Formulación magistral en patología de la mucosa oral. Actas Dermosifiliogr. 2020;111:822–828.