Paraphenylenediamine (PPD) is an amine that is mainly used as an ingredient in hair dyes and henna tattoos. The incidence of allergic contact dermatitis to PPD is increasing, particularly in younger patients. In this article, we review the main sources of PPD and the substances with which it can interact and present a practical algorithm for diagnosing and treating suspected cases of PPD allergy.
La parafenilendiamina (PPD) es una amina empleada en la actualidad principalmente como componente de tintes capilares y en tatuajes de henna. Se ha observado un incremento en la incidencia de la dermatitis alérgica de contacto por PPD, y en edades cada vez más tempranas. En el presente trabajo se realiza una revisión de las principales fuentes que contienen PPD, así como de las sustancias con las que puede interaccionar, y se propone un algoritmo de manejo diagnóstico y terapéutico desde un enfoque práctico, para los pacientes que presenten una clínica compatible con sospecha de alergia a PPD.
Paraphenylenediamine (PPD) is an aromatic amine1 that was synthetized in Germany by Hoffman in 1833 with the aim of developing a substance with good antioxidant and staining properties.2 It is found in various products, including rubbers, printer ink, photographic products, and footwear, although the main sources and those of greatest current relevance are henna tattoos and hair dyes. In the case of hair dye, the molecular characteristics of PPD mean that it provides very good cosmetic results; however, it also penetrates the skin easily, leading to sensitization and subsequent development of allergic contact dermatitis. The prevalence of allergic contact dermatitis caused by PPD in the general population is estimated to be between 0% and 1.5%; in patients who undergo patch tests, this percentage is around 4%.3 Given the use of PPD in hair dye at increasingly younger ages and in henna tattoos for children, the incidence of allergic contact dermatitis to PPD is increasing in general, but especially in children,2,8 even though relevant legislation applies for use of PPD in these practices.12 Consequently, there is a need to make the public aware of the allergenic potential of PPD and to make manufacturers aware of the need to modify the composition of hair dyes through the introduction of less allergenic components.4 Thus, we could reduce the prevalence of allergic contact dermatitis to PPD, which is considered an occupational skin disease in hairdressers.5
In the present article, we review PPD, the products where it is found, the substances it interacts with, its epidemiology, and legal aspects. We also provide proposals on diagnosis and therapy of affected patients with the aim of improving their quality of life and reducing the impact of PPD in the workplace.
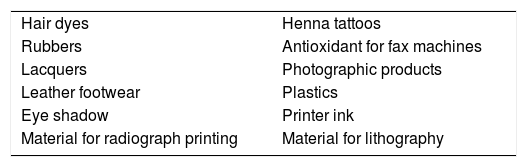
Sources of ParaphenylenediaminePPD has been identified in multiple sources. Table 1 shows the most common and relevant sources.21,23 Of all those shown, the 2 most common sources of PPD are hair dyes and henna tattoos.
The hair dyes we use today first appeared in 1893 and were applied for cosmetic purposes. Since then, more and more people have used them,2 especially women, although they are now increasingly used by men,15 and at younger ages.
PPD is found in permanent dyes, although it is also found in semipermanent and vegetable dyes.
Permanent dyes (2 tubes) contain PPD and other, similar substances. They require a colorant containing PPD and an oxidizing agent, the most common of which is hydrogen peroxide. Both substances are mixed, and the resulting product is applied to the hair. An appropriate mix ensures that PPD is polymerized, thus hampering absorption by the skin and, therefore, subsequent sensitizing capacity.37 While PPD is not the only or most widely used substance, it is very popular because of its favorable cosmetic results and its duration. However, it is also one of the most antigenic substances. A study performed in the USA showed that resorcinol and m-aminophenol were more common than PPD. Other common components of hair dye include p-aminophenol and 2,5-toluenediamine. Yazar et al.12 studied the prevalence of the main sensitizers in 105 hair dyes in Spain and found that 90% contained 4 or more potent allergens and that they all contained at least 1 of these allergens.
Black henna tattoosNatural henna is reddish-brown in color and has very low sensitizing capacity.22 In order to ensure darker coloring that lasts longer, the henna is mixed with other substances, mainly PPD, even though this practice is banned. Adding PPD increases the duration of the pigment in the skin from 2-6hours to 2-6 weeks.23 In developed countries, henna tattoos are placed for recreational purposes, especially in children and adolescents. The concentration of PPD in henna tattoos ranges from 4.28% to 27.24%24; in Spain, concentrations higher than 10% have been reported.25,26 Such high concentrations induce an intense immune response that favors concomitant sensitization to other substances that come into contact with the skin during placement of the tattoo. These substances include colophony (adhesive on dressings) and thiuram mix (rubber gloves worn by the tattooist).23 In addition to the high concentrations of PPD in the tattoos, other factors that favor penetration and sensitization include the following: use of sharp needles and objects, which facilitate penetration of substances across the stratum corneum; the occlusive material placed over the tattoo; and retracing of the tattoo days after placement, with re-exposure to the allergen.23 Henna tattoos with PPD can cause severe reactions that require immediate management and even admission to hospital.23,27 This type of reaction can appear after application of hair dyes; in the case of tattoos, reactions sometimes appear years after placement.28,29
LegislationThe high sensitizing capacity of PPD has led to the drafting of appropriate legislation, which has become stricter over time. In 1976, the maximum concentration of PPD in hair dyes was set at 6%.20 Subsequently, in 2009, the regulation was modified so that the maximum concentration after mixing with the oxidizing agent for direct application on the hair was 2%. In the USA, there is no regulation of the limits for concentrations of PPD in hair dyes.
Furthermore, current European legislation states that PPD cannot be applied directly on the skin, eyebrows, or eyelashes. Therefore, it is banned in both temporary and permanent tattoos.
Molecular Structure of PPD: Cross-reactionsPPD is a hydrophilic aromatic amine with a low molecular weight (108.1kDa) that has a high ability to bind to proteins, thus giving it a considerable capacity for penetrating the skin and a high allergenic potential,9 similar to that of diphencyprone and methylchloroisothiazolinone.1
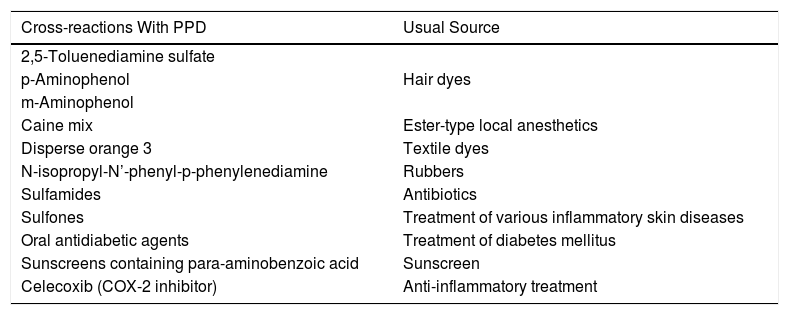
Other substances have a similar structure to that of PPD, which in sensitized patients can produce an allergic reaction without the need for concomitant exposure to PPD (cross-reaction).31
It is important to know which substances cause cross-reaction with PPD (Table 2) in order to make the appropriate recommendations to patients.
Paraphenylenediamine: Cross-reactions.
| Cross-reactions With PPD | Usual Source |
|---|---|
| 2,5-Toluenediamine sulfate | |
| p-Aminophenol | Hair dyes |
| m-Aminophenol | |
| Caine mix | Ester-type local anesthetics |
| Disperse orange 3 | Textile dyes |
| N-isopropyl-N’-phenyl-p-phenylenediamine | Rubbers |
| Sulfamides | Antibiotics |
| Sulfones | Treatment of various inflammatory skin diseases |
| Oral antidiabetic agents | Treatment of diabetes mellitus |
| Sunscreens containing para-aminobenzoic acid | Sunscreen |
| Celecoxib (COX-2 inhibitor) | Anti-inflammatory treatment |
Sensitizing capacity and development of allergic contact dermatitis
PPD is a prehapten whose characteristics enable it to cross the skin barrier easily. It has been detected in plasma, urine, and feces after application of hair dye for 5-30minutes. PPD is also absorbed rapidly, peaking in plasma 2hours after application, and is almost undetectable at 24hours.9
PPD is a very unstable compound owing to the rapid self-oxidation it undergoes on contact with oxygen. Several derivatives of PPD with high allergenic potential have been discovered, although the most important are Brandowski base and benzoquinone.1,9,10,14
These derivatives can stimulate CD8+ and CD4+ T lymphocytes, thus increasing secretion of cytokines that are dependent on type 2 helper T cells.10
In addition to the oxidation phenomenon that favors sensitization, PPD undergoes acetylation by keratinocytes, whose products are not capable of stimulating dendritic cells.10 It is thought that 80% of PPD that penetrates the skin undergoes acetylation. Therefore, although PPD generally becomes inactive, the balance between acetylation and oxidation favors oxidation and can trigger an allergic reaction in some patients.
EpidemiologyPPD is the component of hair dyes that is associated with a greater prevalence of allergic contact dermatitis both in users and in hairdressers.11 The prevalence of allergic contact dermatitis caused by PPD ranges from 0% to 1.5% among the general population in Europe,16 although it is thought to be underdiagnosed.27 A study carried out among the general population in 5 European countries15 revealed a prevalence of 0.8%, and a significant association was recorded between having a henna tattoo and allergic contact dermatitis. In patients who undergo patch tests, this percentage increases to 4% to 5% in Spain, which is similar to that reported in other countries in Europe and Asia and lower than in North America (6%).16,28 A slightly higher prevalence has been reported in females than in males.9,17
Risk Factors for Development of Allergic Contact Dermatitis to PPDA large part of the population are home users of or come into contact with hair dyes on a regular basis; only a percentage of these people become sensitized to PPD. The various factors that favor sensitization can be classified as intrinsic and extrinsic.
Intrinsic risk factorsIt has been postulated that predisposition to sensitization to PPD has a genetic basis. Blömeke et al. observed a greater prevalence of the tumor necrosis factor α genotype GA and AA in patients who were allergic to PPD. In addition, this genotype has been associated with a greater rate of sensitization to various allergens.17,18
Alteration of the skin barrier in patients with atopic dermatitis facilitates the entry of antigens.3 Moreover, production of oxygen free radicals is more pronounced in these patients, resulting in a greater frequency of oxidation of PPD and an increased probability of sensitization.19
Extrinsic risk factors- •
Occupation. Hairdressers more often present with this type of occupational skin disease, since they come into daily contact with dyes.3 Even so, occupational ACD is considered to affect a minority of persons with respect to the total number of cases affected.17 Other professions with a high risk include drivers (rubber steering wheel, leather upholstery, etc.), cleaners, and people who work in printing.18
- •
Hair dye users. The tone of the hair dye can affect the risk of sensitization, since darker tones contain higher concentrations of PPD. One study analyzed this concentration in various Spanish and Swedish dyes and found that PPD was present in 50% of the Spanish dyes and in only 16% of the Swedish dyes. The authors suggested that the darker tones are used more frequently in the south of Europe than in the north.13,32
Sensitization to PPD is time- and dose-dependent.1,35 Application of a hair dye for as little as 5minutes has the potential to trigger an allergic reaction.9 Persons who have no experience of using hair dyes at home usually take longer to apply the dye to the scalp, thus increasing the risk of allergic contact dermatitis.
SymptomsSkin manifestations of allergic contact dermatitis to PPD usually appear 24-72hours after contact in previously sensitized patients and at 4-14 days in cases of first exposure.23
We can differentiate between symptoms triggered by hair dye and those triggered by tattoos.
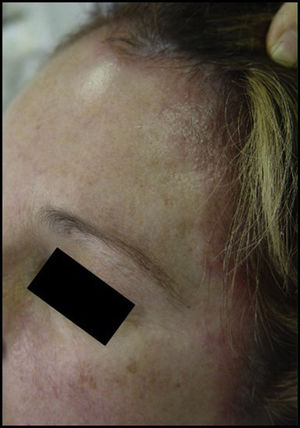
- 1.
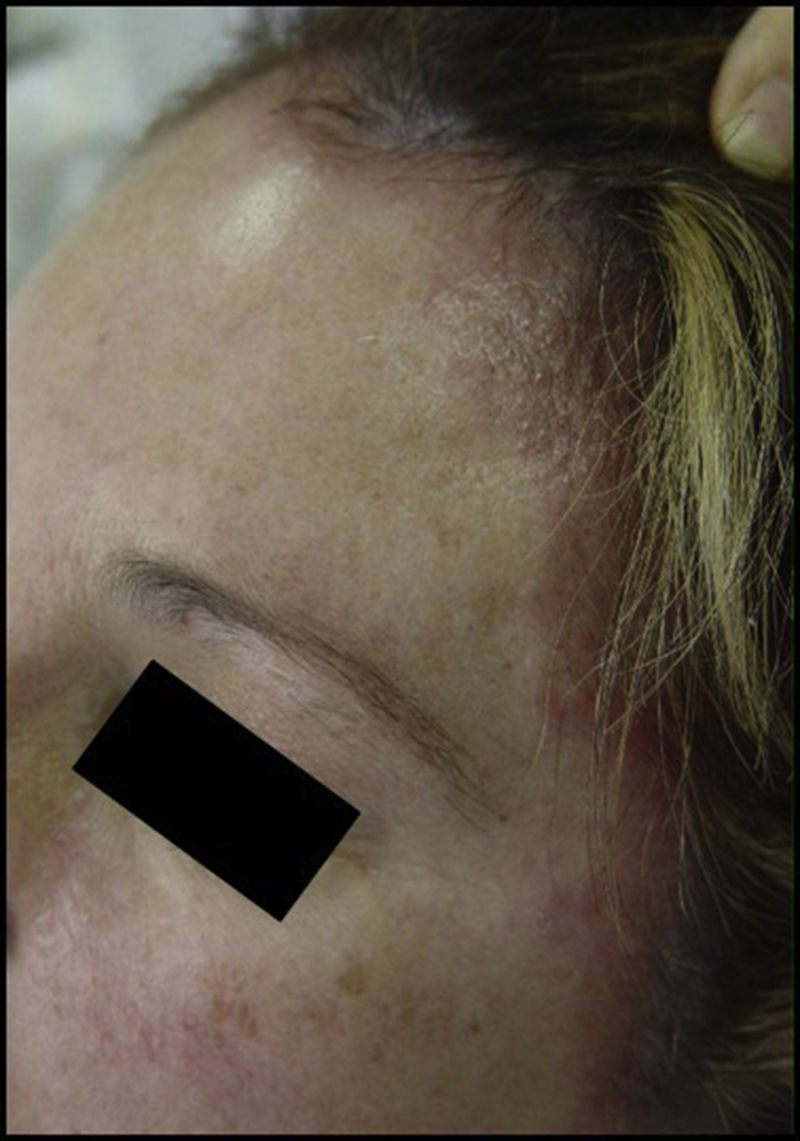
Hair dye. The symptoms are usually very dramatic, taking the form of acute eczema on the scalp, face (mainly forehead and eyelids), and neck (especially the nape and retroauricular area). Exceptional cases of hair loss have been reported (Figs. 1 and 2).
- 2.
Henna tattoos. Acute eczema, generally limited to the area of the tattoo, although there have been reports of cases of generalized eczema and, less frequently, erythema multiforme–type dermatitis.30 In children, henna tattoos commonly cause postinflammatory hypopigmentation, whereas in adolescents and adults, hyperpigmentation is more common. Both hypopigmentation and hyperpigmentation usually last for at least 6 months, although they can be permanent23 (Fig. 3).
- 3.
Hairdressers. The reaction takes the form of chronic hand eczema (Fig. 4).
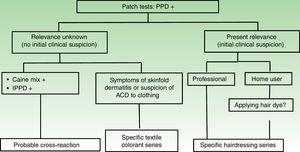
The clinical history, symptoms, and location of the lesions are the main factors that guide us toward a diagnosis. Patch testing must always be performed in cases of suspected allergic contact dermatitis to PPD (Fig. 5). PPD is a good marker of allergy to hair dyes and is included in standard series and in the T.R.U.E. TEST series. The concentration of PPD is 1% in petrolatum in the standard series and somewhat less in the T.R.U.E. TEST (90μg/cm2).2 A concentration of 0.3% is thought to be sufficient,34 especially in children and in patients who experience severe reactions to a dye or tattoo ink. There have been isolated reports of active sensitization after patch testing.31
Patch test reading at 96hours in a patient with suspected allergy to paraphenylenediamine. Positive results were found for paraphenylenediamine, N-isopropyl-N-phenyl-paraphenylenediamine, benzocaine, and various components of the hairdressing series as a probable consequence of cross-reaction.
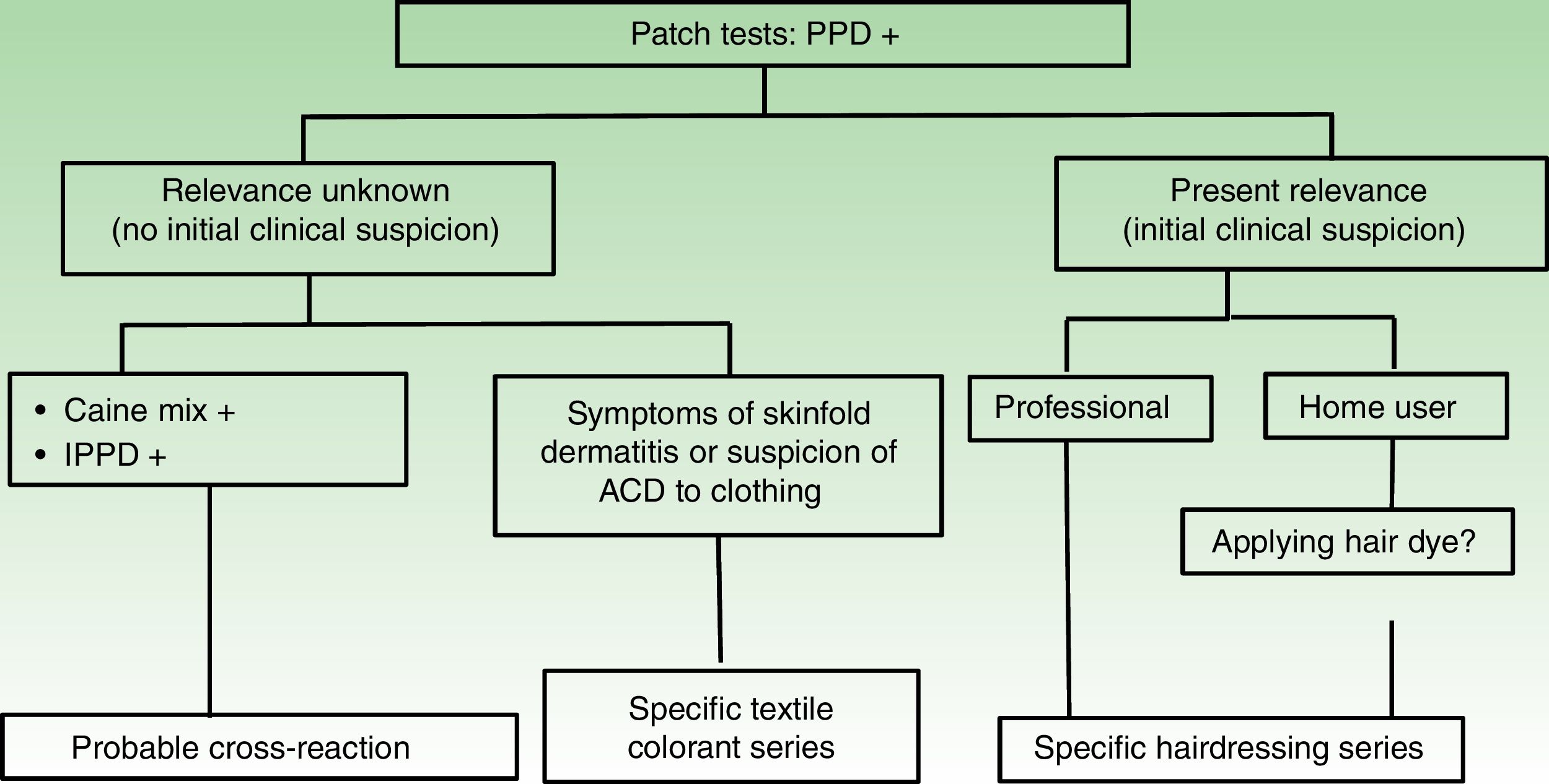
The algorithm (Fig. 6) makes a proposal for the diagnosis of patients with positive patch test results to PPD. In the case of an initial clinical suspicion of allergic contact dermatitis to dyes and negative patch test results, the dermatologist should question the patient again and consider the possibility of irritant contact dermatitis or another disease with a similar clinical presentation, such as psoriasis or seborrheic eczema.2,7
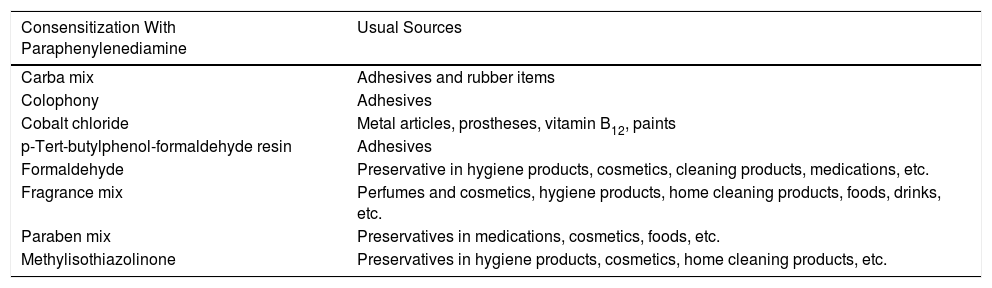
Patients who are allergic to PPD, especially in chronic and occupational cases, are usually sensitized to multiple substances, most of which are present in work-related objects (eg, gloves, scissors) or in hygiene and cosmetic products. Table 3 shows the most frequent cosensitizations for PPD.6
Paraphenylenediamine: Main Cosensitizationsa
| Consensitization With Paraphenylenediamine | Usual Sources |
|---|---|
| Carba mix | Adhesives and rubber items |
| Colophony | Adhesives |
| Cobalt chloride | Metal articles, prostheses, vitamin B12, paints |
| p-Tert-butylphenol-formaldehyde resin | Adhesives |
| Formaldehyde | Preservative in hygiene products, cosmetics, cleaning products, medications, etc. |
| Fragrance mix | Perfumes and cosmetics, hygiene products, home cleaning products, foods, drinks, etc. |
| Paraben mix | Preservatives in medications, cosmetics, foods, etc. |
| Methylisothiazolinone | Preservatives in hygiene products, cosmetics, home cleaning products, etc. |
- 1.
Treatment of acute manifestations. Depending on the severity of the reaction, topical and/or systemic corticosteroids can be prescribed. The patient should be advised to avoid contact between the hair and the skin, through measures such as haircutting or washing his/her hair with the head held back.
- 2.
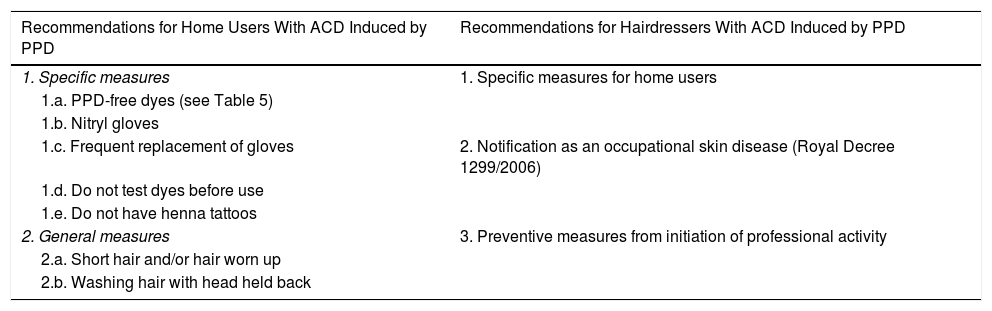
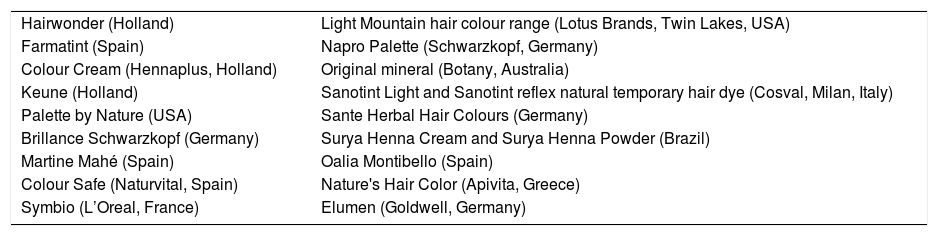
Preventive measures. It is sometimes difficult to make the patient aware of the importance of avoiding the allergen, especially in cases where the reaction is mild.3Table 4 lists preventive measures for both users and professionals.38,39Table 5 provides a list of dyes that do not contain PPD, which should prove useful for those patients who are sensitized or allergic to this substance.
Table 4.Recommendations for Users of Paraphenylenediamine and Hairdressers.
Recommendations for Home Users With ACD Induced by PPD Recommendations for Hairdressers With ACD Induced by PPD 1. Specific measures 1. Specific measures for home users 1.a. PPD-free dyes (see Table 5) 1.b. Nitryl gloves 1.c. Frequent replacement of gloves 2. Notification as an occupational skin disease (Royal Decree 1299/2006) 1.d. Do not test dyes before use 1.e. Do not have henna tattoos 2. General measures 3. Preventive measures from initiation of professional activity 2.a. Short hair and/or hair worn up 2.b. Washing hair with head held back Abbreviation: ACD, allergic contact dermatitis; PPD, paraphenylenediamine.
Table 5.Paraphenylenediamine-Free Dyesa
Hairwonder (Holland) Light Mountain hair colour range (Lotus Brands, Twin Lakes, USA) Farmatint (Spain) Napro Palette (Schwarzkopf, Germany) Colour Cream (Hennaplus, Holland) Original mineral (Botany, Australia) Keune (Holland) Sanotint Light and Sanotint reflex natural temporary hair dye (Cosval, Milan, Italy) Palette by Nature (USA) Sante Herbal Hair Colours (Germany) Brillance Schwarzkopf (Germany) Surya Henna Cream and Surya Henna Powder (Brazil) Martine Mahé (Spain) Oalia Montibello (Spain) Colour Safe (Naturvital, Spain) Nature's Hair Color (Apivita, Greece) Symbio (L’Oreal, France) Elumen (Goldwell, Germany)
Current research is focused on dyes containing methoxy methyl-paraphenylenediamine (PPD derivative), which causes reduced activation of the innate and adaptive immune systems, with very good cosmetic outcomes.36 Ascorbic acid has also been proposed as pretreatment for exposure to PPD owing to its antioxidant properties.33
ConclusionsPPD is a potent allergen that is involved in allergic contact dermatitis associated with hair dyes and tattoos. Knowledge of this condition is important in order to diagnose it early and make patients aware of the need to take preventive measures. In this way, we will be able to reduce the potential impact of this condition on the quality of life of both home users and professional users, especially hairdressers.
Conflict of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Durán BE, Romero-Pérez D, Salvador JFS. Actualización en la dermatitis de contacto alérgica por parafenilendiamina. Actas Dermosifiliogr. 2018;109:602–609.